Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Perhaps one of the most researched topics is ACL injuries. I have been studying and working for years in my clinical practice to find the best ways to rehab athletes following injury as well as implement the most effective injury prevention strategies. Prior studies indicate prevention programs even when self directed can be successful.
However, on the whole injury rates have not declined over the past decade or so. Much attention has been given to valgus landing mechanics, poor muscle firing, stiff landings, genetic difference between males and females, ligament dominance, quad dominance, and so forth. The predominant thoughts today for prevention center around neuromuscular training and eliminating faulty movement patterns (refer to work being done by Timothy Hewett and Darin Padua).
We also know from a biomechanical standpoint that the hamstrings play an integral role in preventing excess anterior tibial translation, and as such hamstring strengthening needs to be a big part of the rehab and prevention program. I believe in hamstring training that allows for activation in non-weaightbearing and weight bearing positions. Common exercises I will use include:
- HS bridging patterns (double /single leg, marching, knee extension, stability ball)
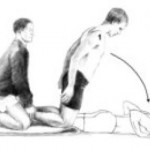
- Nordic HS curls
- HS curls (stability ball, TRX or machine)
- Sliders – focus on slow eccentric motion moving into knee extension followed by simultaneous curls/bridge
- Single leg RDL (add dumbbells or kettle bells for more load)
Note: click on any of the thumbnail images above for a full view of the exercise. From left to right: Nordic HS curls, sliding hamstring curls and single leg RDL).
A recent blog post entry by the UNC Department of Exercise and Sport Science (@UNCEXSS) has spurred my post today. Click here to read their entry on optimizing injury prevention based on work done by Professor Troy Blackburn regarding the effect of isometric and isotonic training on hamstring stiffness and ACL loading mechanisms. The research that was done holds promise for hamstring training designed to increased musculotendinous stiffness (MTS).
I had the pleasure of listening to Darin Padua, PhD, of UNC present some of his latest research on ACL injury prevention last week. He has been doing research for some time. One of his studies (JUMP ACL) in collaboration with the military and several others has looked at prospective data and injury occurrence among college age subjects.
Much of the research to date on injury prevention has been done by Timothy Hewett and his colleagues. It has concluded that drop landing with a valgus collapse (hip abduction/IR with valgus knee moment) is a risk factor for injury. Interstingly enough, despite that knowledge and the proliferation of prevention programs, Darin mentioned that overall these prevention programs have not slowed the rate of ACL tears in the last decade. Why is that? He also relayed that much of what we know now is based on 15 total cases.
The Jump ACL Study in a nutshell lasted for 5 years at 3 different military academies:
N = 5,700 cadets with no prior ACL surgery
- Soccer players = 1,690
- Tested from 2005 to 2008
- 39% female; 25% NCAA athletes
- 14,653 person-years of follow-up
N = 113 incident ACL injuries
- Soccer players = 29
- Mean time from testing to injury = 3.1 yrs
- N = 92 one ACL injury; N = 11 two ACL injuries
Some data (will be published) he discussed based on his findings revealed the following about high risk profiles for ACL injury:
- Hip flexion > 40 degrees at landing = 1.76x increased risk
- Hip adduction plus knee valgus = 3x increased risk
- Hip adduction plus knee varus = 27x increased risk
He also mentioned that the high risk profile does not correspond to the ACL injury event profile of:
- Hip abduction
- Lateral trunk flexion
- Knee valgus collapse
- Small knee flexion
- Tibial ER/IR
In the end, he suggests we need to better understand who to target (high risk profile clients) and what to modify (injury event profile) so we can better customize injury prevention programs that optimize proper movement and meet the needs of each individual athlete. He reminded us that using the uninjured side for comparison is insufficient as faulty movement patterns already likely existed contributing to the first ACL injury.
So, assessing movement continuously and striving for excellent movement quality is a MUST if we are going to both prevent initial ACL injuries and reduce the re-tear rates for our athletes we send back to play. He reports that those at increased risk simply have bad biomechanics. His message provides more weight to having an advanced algorithm to identify asymmetry, poor motor control and flawed movement patterns in order to effectively prescribe interventions to address these things.
At UNC they use a PRIME assessment. I am excited to learn more about it and have referred one of my female higher level soccer players to their lab for assessment as I look at this return to play decision with her now that she is just past 7 months post-op. I think the hip/core obviously play an important role as I see so much deficiency in my female patients recovering from injury.
Clearly his findings with hip adduction and varus as a big risk factor seem to indicate it could be a top down kinetic chain breakdown as well upon impact based on the risk profile. Pelvic stability or the lack thereof seems to be significant, only NOT in the same manner we thought about it before based on previous research available. Stay tuned, as we have lots more to learn about ACL injuries and how best to tailor our prevention efforts.
Knowing just when to put an athlete back on the field after ACL reconstruction is a difficult proposition. Surgeons often look at swelling , graft stability and quad girth. In the past, we have relied on isokinetic testing and hop testing measures in the clinic as guidelines as well.
As a sports performance specialist and clinician, I am keenly interested in not only fully rehabbing this injury, but also preventing it form happening again in the future. Observing quality of movement in cutting, jumping, running and drills offers good insight in this process, but I think we need more.

The FMS and Y-Balance test are things I use in my equation as well. I often see clients ace the YBT, but struggle to obtain a passing score on the FMS based on issues in core stability and the deep squat. Current literature reports that any score less than a 14 carries a 4-fold increase for non-contact injury risk in female collegiate athletes. Click here to read that study.
In addition, I look at the following for return to play decision making:
- Single leg squat depth
- Single leg broad jump
- Single leg impact mechanics
- Deceleration and cutting form
- Cross-over hop test
- Single leg triple hop
- 6 M timed hop test
Below is a video of the single leg broad jumps, the triple hop, cross-over hop test and 6 M timed hop test.
What does research have to say? I think we have a vacuum where athletes get “cleared” or released from PT and they wonder back to sport too soon.
Continue reading…
It is widely accepted that decreased hip strength and stability leads to knee valgus. Excessive frontal plane motion and valgus torque increase the risk for non-contact ACL injuries. While we know that hip abductor weakness is more of an issue in females than males, the question remains to what degree other factors are involved.

Claiborne et al (1) noted that only 22% of knee variability could be linked solely to hip muscles surrounding the hip. In light of this we must look at the whole kinetic chain when assessing movement dysfunction and injury risk. In the most recent issue of the IJSPT, researchers sought to discover how activating the core during a single leg squat would impact the kinematics of 14 female college-age women. They excluded participants with current pain or injury to the lower extremities or torso, or if they had a history of any lower extremity injuries or surgeries in the past 12 months.
The participants were assessed for their capacity to recruit core stabilizer muscles using lower abdominal strength assessment as described by Sahrman (2). This testing model has 5 levels of increasing difficulty used to challenge participants to maintain a neutral spine. The draw back of this method is that it is done in supine versus the standing position of this study, but the author acknowledges this limitation. Out of a possible high score of 5, five of the participants scored a 1 or 2, while the other nine scored a zero.
For the study, a six inch step was used to assess 2 reps of a single leg squat. Each participant was asked to perform the test with the dominant leg to standardize conditions. They performed the reps under two conditions:
1. CORE – engaged abdominal muscles as they had been instructed to do so during the Sahrman test
2. NOCORE – no purposeful engagement of abdominal muscles
Results
- The CORE condition resulted in smaller hip displacements in the frontal plane but had no effect on hip angular range of motion – essentially there was less medial/lateral movement
- The CORE group did not exhibit any changes in knee displacement but did exhibit greater degree of knee flexion – this may suggest higher function assuming more knee flexion is desired during squat tasks in sports and functional activities
- Those scoring the lowest on the core assessments had larger improvements in performance when they did in fact activate the core musculature
How do we use this information to affect our practice? Well, in terms of rehab it seems straightforward and many of us may already encourage patients to activate their core during treatment. However, I think the greater contribution may come in injury prevention programs (particularly ACL programs) where we are looking at all facets of neuromuscular control and appropriate muscle activation patterns.
With any prehab or rehab strategy, we as clinicians, trainers and strength coaches are essentially trying to reprogram the brain to summon and execute a better motor pattern or strategy – feedforward training. We know that healthy individuals tend to have better transverse abdominus and multifidus muscle activation, so it only makes sense to consider activation of local stabilizers as we work on global muscles. Improving core and pelvic stability should only help reduce unwanted frontal plane motion.
With that said, the authors of this study readily acknowledge more work needs to be done with larger clinical populations (including EMG work) to more clearly identify what magnitude the core musculature has on lower extremity motion and displacement.
Keep in mind the proper program will always stem from your ability to assess movement impairment and tissue dysfunction. I suggest beginning with a FMS in the athletic population and incorporating parts of that or the SFMA to compliment your evaluation in the clinic. This will generally reveal the priorities for the corrective exercises. For now, we can use this information in this particular study to be more intentional with our patients and clients suffering knee and hip dysfunction by adding this one simple step to our programming.
References
1. Claiborne TL, Armstrong CW, Gandhi V, Princivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. Journal of applied biomechanics. 2006;22(1):41.
2. Faries MD, Greenwood M. Core training: stabilizing the confusion. Strength & Conditioning Journal. 2007 ;29(2):10.
I just finished presenting at our our second ACL Symposium of the year at the Athletic Performance Center last Saturday. Rehabbing and training female athletes has been a passion of mine for some time. Over the years, I have also developed a love for research and reading it, particularly studies on the ACL.
In my practice, I have incorporated jump landing, single leg training and deceleration based training for some time. While we all know females are 3-8 times more likely to suffer an ACL injury than males, we have not isolated the exact reason why. Researchers have offered some clues such as: wider pelvis, narrow femoral notch, smaller ACL, ligament dominance, limb dominance, natural laxity (hormonal factors), wider Q angles, and faulty muscle firing patterns to name a few.
Many of the structural factors are beyond our control. So, as practitioners, we must focus on the training. Consider the following study just published in the August 2011 edition of the American Journal of Sports Medicine that basically reveals females develop peak valgus moments during deceleration during a drop landing maneuver, whereas males develop peak valgus forces during acceleration on the way back up:

Drop Landing
This article adds more evidence that females recruit and fire their muscles very differently than males. More importantly, it reiterates that we as coaches, therapists and S & C professionals need to be working on deceleration mechanics. I believe this starts with simple soft two legged drills such as:
- Small squat jump and holds
- Box drops and holds
- Forward line jump, stick and hold
- Lateral line jump, stick and hold
- 90 degree jump turn, stick and hold
In addition, one of my favorite drills is a single leg forward leap (hop) and stick working on deceleration. The athlete stands on the right leg and then pushes off forward landing on the left leg. Coaching the athlete to land softly on a bent hip and knee while avoiding valgus is important. I usually perform 2-3 sets of 5 reps on each side. Cueing with a mirror, auditory corrections and tactile cues are useful in encouraging proper form.

SL Stick (start)

SL Stick (finish)
It is important to keep in mind that the majority of non-contact ACL tears occur between 0 and 30 degrees of knee flexion. They also typically involve deceleration (landing, jump stop or change of direction), planting or cutting. For this reason, deceleration training must also involve programming for agility and change of direction.
On Saturday, I led the break-out session on deceleration training and covered a few key exercises I use with my athletes. These drills are layered on one another and the basic ones I begin with are:
- Stops – I have athletes accelerate out and then decelerate to a controlled two legged stop after 10-20 yards. Keep in mind allowing for a longer run will allow the athlete to gradually slow down, while decreasing the distance increases intensity and force on the knees. I coach breaking down with small “pitter patter” steps versus a sudden hard stop.
- 2 cone lateral shuffle stops – the athlete shuffles over 5-6 yards and then stops with good hip, knee and foot alignment working to keep the shoulders inside the knees (inside the box). I progress to multiple cone shuffles to increase intensity and maximize repetitive deceleration.
- Pro-agility drills – 3 cones are placed 5 yards apart and I combine linear and lateral movements between the cones layering #1 and #2 above in a continuous pattern to work on acceleration/deceleration combos and change of direction
- Y drill (4 cones) – the athlete runs forward to a cone 5-15 yards out and then performs a 45 degree cut left/right. The progression begins with directed and predictable movement and then advances to reactive cueing with auditory and visual cues.
- Arrow drill (4 cones) – The athlete runs 5-15 yards forward and then performs a 135 degree cut left/right and runs past the cone that serves as the bottom edge of the arrow head. This is much more demanding on the body (knee) and as such I only move to this after the Y drill has been mastered. In addition, I teach a hip turn (from Lee Taft) to reposition the hips and minimize torsion on the lower leg. I move from predictive to reactive agility as in the Y drill.
These exercises are a small sampling of my ACL prehab/rehab routine. I also include an enormous amount of single leg PRE’s and balance training as well. I believe the most important things we can currently do to reduce ACL risk in this population are:
- Screen our athletes to help identify risk (FMS, drop landing, dynamic strength,running/cutting analysis)
- Emphasize hamstring, gluteus medius and lateral rotator strengthening
- Teach landing mechanics and proper deceleration through neuromuscular exercise, biofeedback and repetitive cueing
- Refine proper cutting technique by teaching ideal angles and how to reposition the hips
- Empower coaches and athletes with simple yet effective body weight training routines that can be replicated on the field or court with the team
For now, the battle rages on. I hope you will join me in the quest to prevent these catastrophic injuries. I think as research evolves we will continue to see that the answer to promoting optimal stability at the knee will increasingly have more to do with addressing the hip and ankle. For now, we need to teach soft bent knee landing/cutting that shifts the body’s center of mass forward, while eliminating valgus loading as much as possible in the danger zone.