Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Over the past several years, the trend in the health and fitness industry has been toward injury prevention and movement screening. Gray Cook and Lee Burton have given us the FMS. More recently, the Y-Balance test has emerged as another tool to assess asymmetry in the upper and lower quarter.
I am currently FMS certified and planning to attend the SFMA course next month in Durham. I routinely incorporate the FMS in both our rehab and sports performance work at the APC. I like many things about the screening exam. It provides a consistent tool to assess baseline movement and record asymmetry on a simple 4 point scale scale. It also has been shown to have good intra and inter-rater reliability. Click here for a recent study published in the Journal or Orthopaedic & Sports Physical Therapy.
For those unfamiliar with the screen, it is 7 tests scored on a 0-3 scale as follows:
- 0 = pain
- 1 = unable to perform the movement pattern (or perform with marked dysfunction)
- 2 = performs the movement with a mild compensation
- 3 = performs the movement correctly
I would say on average, most of the athletes I screen score between a 12 and 15. My highest score was a 19 (9 year old gymnast) and my lowest was a 9 (NFL lineman). As screeners, we are charged with uncovering asymmetry and faulty movement patterns. What do you see in the following picture?

Clearly, the dowel is not level, thus we score it a 2. She also had some ER in the right leg when stepping over the hurdle. She was a symmetrical 2 on the hurdle step test. This is a Division I soccer player who scored 17 on the exam.
Most of the movements seem straightforward. However, many question what the rotary stability test measures with respect to the ideal 3 score (ipsilateral movement)? It assesses an unnatural movement pattern to be sure. This athlete failed miserably on the ipsilateral pattern but scored a solid 2 with the contralateral pattern.

I have yet to test someone who can score a legitimate 3. I have seen some get a 3 on one side and 2 on the other (asymmetrical and a red flag in FMS land). As one who naturally questions things, I find myself questioning how many are truly capable of scoring a 3.
Disclaimer: This post is a small rant from me. I normally don’t use this blog as a medium for that purpose. However, I feel so strongly about this topic that I decided to share my thoughts on it.

I had an interesting email exchange with a health care practitioner (HCP) this past week. She had some questions about one of my products and asked specifically if I had done a clinical trial comparing my treatment method to leading national PT organizations. My answer was no.
I explained to her I am not a researcher, nor do I have the time (or money for that matter) for such things as I am in the trenches every day treating patients and training athletes. Her response was very interesting. According to her I was defensive, and she suggested I check out a DPT program so I could in essence become a better clinician.
Hmmm……… Suffice it to say I completely disagree with her on this one. I graduated from PT school at the Ohio State University in 1996. Their program was very well respected at the time (over 500 applied and they took 60 in my class) and two of my professors (Lynn Colby and Carolyn Kisner) wrote the text on Therapeutic Exercise that is still used in many curriculums today. On top of that, I worked at the top outpatient ortho clinic in the city as an aide my junior and senior year in college.
At the time of my admission, OSU only offered a B.S. degree, so I never had a choice for more at that point. The university quickly adopted a Master’s program shortly after I finished and later became one of the first institutions to offer the full DPT program.
Upon graduation, I went to work at the same top ortho clinic and spent 5 years working side-by-side with some of the brightest PT’s and next door to what was considered by many to be the best surgical group in town. I saw surgeries, sat in on MD appointments with my patients, participated in journal clubs and worked at a feverish pace. Let’s just say I saw lots of patients and gained what felt like a fellowship experience for 5 more years.
Now, as I reflect upon this email from said HCP, I can honestly say that I believe experience and results matter more than just those three letters behind a name. That is in no way meant as a slam or any disrespect to the DPTs out there, clinical research trials or the doctorate degree itself. Students today have no choice but to take the DPT route. To be honest, they really only have (1) more year of structured curriculum than I had in my program. They leave school with a lot more debt, and afterward they still have no clinical (real world) experience when they first start out. You simply can’t buy experience in school.
Research along with years of observation has taught me that the brain is inherently looking for the most efficient way (aka least effort) to execute movement in life. In addition, it HATES pain just like you and I so it does everything possible to avoid it including ordering the body to perform dysfunctional movement patterns.
After a painful episode, the brain often needs reminded that the body can go back to the proper movement patterns once the pain is gone. However, it often holds that painful memory and may by default lean toward a faulty movement pattern. This protective mode then ends up perpetuating a faulty movement pattern that is no longer necessary nor efficient. Over time, dysfunctional movement patterns can create further stress or harm to other segments in the kinetic chain.
So, I am always seeking ways to stimulate the body to work properly and exercises that facilitate proper neuromuscular patterning are instrumental in my rehab and training. I wanted to share two exercises that I like to utilize in my rehab and training for the shoulder. In particular, I like to employ closed chain activity to stimulate the serratus anterior as well as the other scapular stabilizers.
Below are two exercises I wrote about in my “Functionally Fit” column for PFP magazine. The first exercise shows quadruped rocking. Shirley Sahrmann mentions this in her work, Diagnosis and Treatment of Movement Impairment Syndromes. I began using it after reading her book, and I agree that it works very well for scapular dysfunction. Below is the start and finish position for the quadruped version as well as my own advanced tripod version of the exercise.
- Quadruped start
- Quadruped finish
- Tripod finish
For a complete explanation of the exercise and its application, click here to read the column.
As a follow-up to this exercise, I included an unstable progression I like to employ using the BOSU trainer. I call this the unstable tripod scapular clock. It can be done on the knees or up on the toes. I have included a quick video on this below. Again, I like this exercise for scapular work as well as core stability training.
Click here to read my PFP column on this exercise for the full description, application and regressions. The real beauty of this last exercise is the “big bang for your buck” attributes since it hits shoulder, core and hip stability all at once for those able to work at that level. I hope it works as well for you as it has for me!
There seems to be consistent questions, debate and studies done with respect to stretching. As the thought of more closely analyzing the quality of movement (FMS, Y-Balance testing, SFMA for example) moves to the forefront in the PT and fitness world, many search for the right mix of exercise to maximize mobility.
I count myself as a supporter and follower of the work of Gray Cook and Stuart McGill. While I may not agree 100% with all of their ideas, I generally consider them to be brilliant minds and ahead of the curve. I have been using the FMS in my practice for some time now and have also begun to incorporate Y-Balance testing as well (see pic below courtesy of the IJSPT)
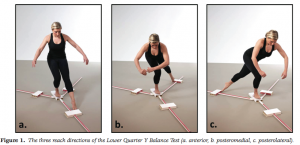
The Y-Balance test may not have significant relevance to hip mobility as much as it does limb symmetry, but I included it here to illustrate my point in observing kinetic chain movement to help determine where the weak link or faulty movement pattern may be. It gives us valuable information with respect to strength, balance and mobility.
With the revelation that FAI is more prevalent than we knew (click here for my post on FAI), I am always interested in hip mobility and how to increase movement in the hip joint. Limitations in hip mobility can spell serious trouble for the lumbosacral region as well as the knee.
I currently use foam rolling, manual techniques, dynamic warm-up maneuvers, bodyweight single leg and hip/core disassociation exercises and static stretching to increase hip mobility. However, I am often faced with the question of what works best? Is less more? How can I make the greatest change without adding extra work and unnecessary steps?
Well, Stuart McGill and Janice Moreside just published a study in the May 2012 Journal of Strength & Conditioning Research that sought to examine three different interventions and how they improve hip joint range of motion. Previous work has been focused on the hip joint alone, and they wanted to see how other interventions impacted the mobility of the hip. Click here for the abstract
So, I treat a number of fitness enthusiasts in the clinic and many include Crossfit clients. Recently, I evaluated a 38 y/o male on 2/16/12 with a 3 month history of right shoulder pain. He performs Crossfit workouts 6 days per week. His initial intake revealed:
- Constant shoulder pain that worsens with overhead movements
- Pain with bar hangs, overhead squats and wide grip snatches
- Unable to do kipping (only doing strict form pull-ups)
- Pain if laying on his right side at night
- No c/o neck pain, referred pain or numbness/tingling
Notice the shoulder position during the kipping pull-up and overhead squat below. This is a position of heightened risk for the shoulder.
His exam revealed the following:
- Normal range of motion
- Strength within normal limits except for supraspinatus and external rotation graded 3+/5 with pain
- Positive impingement signs
- Negative shrug sign
- Negative Speed’s and O’Brien’s test
- Tender along distal supraspinatus tendon
Based on the clinical exam, it was apparent he had rotator cuff inflammation and perhaps even a tear. Keep in mind he had not seen a physician yet. I began treatment focused on scapular stabilization and rotator cuff strengthening as well as pec and posterior capsule stretching to address the impingement. Ultrasound and cryotherapy were used initially to reduce pain and inflammation.
One month following the eval
By 3/14/12, his pain was resolved with daily activity and he had returned to snatches and push-press exercises without pain. He still could not do overhead squats with the Olympic bar pain free, but he could with a pvc pipe. Strength was now 4/5 for supraspinatus and 4+/5 for external rotation. All impingement tests were now negative as were Speed’s and O’Brien’s testing.







