Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Well, Thanksgiving is upon us in 2011. I want to wish you and your family a wonderful holiday. In today’s post I will review a November 2011 article in the American Journal of Sports Medicine that looked at the effect of the Nordic hamstring exercise on hamstring injuries in male soccer players.
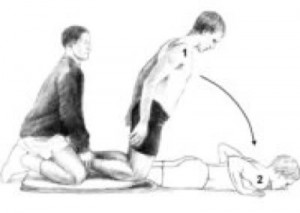
For those not familiar with Nordic hamstring exercises, see the photo below:
In this randomized trial, the researchers had 54 teams from the top 5 Danish soccer divisions participate. They ended up with 461 players in the intervention group (Nordic ex) and 481 players in the control group. The 10 week intervention program was implemented in the mid-season break between December and and March because this was “the only time of the year in which unaccustomed exercise does not conflict with the competitive season.
The trial was conducted between January 7, 2008 and December 12, 2008 with follow-up of the last injury until January 14, 2009. In the intervention group, all teams followed their normal training routine but also performed 27 sessions of the Nordic hamstring exercises in a 10 week program (as follows)
- Week 1 – 2 x 5
- Week 2 – 2 x 6
- Week 3 – 3 x 6-8
- Week 4 – 3 x 8-10
- Weeks 5-10 – 3 sets, 12-10-8 reps
- Weeks 10 plus – 3 sets 12-10-8 reps
The athletes were asked to use their arms to buffer the fall, let the chest touch the ground and immediately get back to the starting position by pushing with their hands to minimize the concentric phase. The exercise was conducted during training sessions and supervised by the coach. The teams were allowed to choose when in training it was done, but they were advised not to do it prior to a proper warm-up program.
And the results…..
I just finished presenting at our our second ACL Symposium of the year at the Athletic Performance Center last Saturday. Rehabbing and training female athletes has been a passion of mine for some time. Over the years, I have also developed a love for research and reading it, particularly studies on the ACL.
In my practice, I have incorporated jump landing, single leg training and deceleration based training for some time. While we all know females are 3-8 times more likely to suffer an ACL injury than males, we have not isolated the exact reason why. Researchers have offered some clues such as: wider pelvis, narrow femoral notch, smaller ACL, ligament dominance, limb dominance, natural laxity (hormonal factors), wider Q angles, and faulty muscle firing patterns to name a few.
Many of the structural factors are beyond our control. So, as practitioners, we must focus on the training. Consider the following study just published in the August 2011 edition of the American Journal of Sports Medicine that basically reveals females develop peak valgus moments during deceleration during a drop landing maneuver, whereas males develop peak valgus forces during acceleration on the way back up:

Drop Landing
This article adds more evidence that females recruit and fire their muscles very differently than males. More importantly, it reiterates that we as coaches, therapists and S & C professionals need to be working on deceleration mechanics. I believe this starts with simple soft two legged drills such as:
- Small squat jump and holds
- Box drops and holds
- Forward line jump, stick and hold
- Lateral line jump, stick and hold
- 90 degree jump turn, stick and hold
In addition, one of my favorite drills is a single leg forward leap (hop) and stick working on deceleration. The athlete stands on the right leg and then pushes off forward landing on the left leg. Coaching the athlete to land softly on a bent hip and knee while avoiding valgus is important. I usually perform 2-3 sets of 5 reps on each side. Cueing with a mirror, auditory corrections and tactile cues are useful in encouraging proper form.

SL Stick (start)

SL Stick (finish)
It is important to keep in mind that the majority of non-contact ACL tears occur between 0 and 30 degrees of knee flexion. They also typically involve deceleration (landing, jump stop or change of direction), planting or cutting. For this reason, deceleration training must also involve programming for agility and change of direction.
On Saturday, I led the break-out session on deceleration training and covered a few key exercises I use with my athletes. These drills are layered on one another and the basic ones I begin with are:
- Stops – I have athletes accelerate out and then decelerate to a controlled two legged stop after 10-20 yards. Keep in mind allowing for a longer run will allow the athlete to gradually slow down, while decreasing the distance increases intensity and force on the knees. I coach breaking down with small “pitter patter” steps versus a sudden hard stop.
- 2 cone lateral shuffle stops – the athlete shuffles over 5-6 yards and then stops with good hip, knee and foot alignment working to keep the shoulders inside the knees (inside the box). I progress to multiple cone shuffles to increase intensity and maximize repetitive deceleration.
- Pro-agility drills – 3 cones are placed 5 yards apart and I combine linear and lateral movements between the cones layering #1 and #2 above in a continuous pattern to work on acceleration/deceleration combos and change of direction
- Y drill (4 cones) – the athlete runs forward to a cone 5-15 yards out and then performs a 45 degree cut left/right. The progression begins with directed and predictable movement and then advances to reactive cueing with auditory and visual cues.
- Arrow drill (4 cones) – The athlete runs 5-15 yards forward and then performs a 135 degree cut left/right and runs past the cone that serves as the bottom edge of the arrow head. This is much more demanding on the body (knee) and as such I only move to this after the Y drill has been mastered. In addition, I teach a hip turn (from Lee Taft) to reposition the hips and minimize torsion on the lower leg. I move from predictive to reactive agility as in the Y drill.
These exercises are a small sampling of my ACL prehab/rehab routine. I also include an enormous amount of single leg PRE’s and balance training as well. I believe the most important things we can currently do to reduce ACL risk in this population are:
- Screen our athletes to help identify risk (FMS, drop landing, dynamic strength,running/cutting analysis)
- Emphasize hamstring, gluteus medius and lateral rotator strengthening
- Teach landing mechanics and proper deceleration through neuromuscular exercise, biofeedback and repetitive cueing
- Refine proper cutting technique by teaching ideal angles and how to reposition the hips
- Empower coaches and athletes with simple yet effective body weight training routines that can be replicated on the field or court with the team
For now, the battle rages on. I hope you will join me in the quest to prevent these catastrophic injuries. I think as research evolves we will continue to see that the answer to promoting optimal stability at the knee will increasingly have more to do with addressing the hip and ankle. For now, we need to teach soft bent knee landing/cutting that shifts the body’s center of mass forward, while eliminating valgus loading as much as possible in the danger zone.
ACL injuries continue to proliferate among female athletes. I am passionate about preventing them, and part of my professional mission is to study and evolve in my rehab and prevention training approaches all the time to stay on top. I wanted to pass along some new information on a new screening tool just unveiled in the Strength and Conditioning Journal this month.
Before I reveal the screening and training tool, I want to take a moment and review what Timothy Hewett refers to as modifiable risk factors that contribute to injury risk based on his work:
- Ligament Dominance – defined as an imbalance b/w neuromuscular and ligamentous control of dynamic knee stability and it is visualized by loss of frontal plane control with landing and cutting
- Quadriceps Dominance – defined as an imbalance between quad and hamstring strength, recruitment and coordination
- Leg Dominance – defined as an imbalance between the two legs with respect to strength, coordination and control
- Trunk Dominance ‘Core’ Dysfunction – defined as an imbalance b/w the inertial demands on the trunk and its ability to resist or control/resist it
Previously, Hewett has identified that high knee abduction moments are related to high LOAD on the knee and a major risk factor for ACL injury. He and his colleagues have done extensive motion analysis in their lab in Cincinnati, OH. As such, a drop landing test has been used as one tool to observe landing mechanics and assign some risk value to athletes competing in cutting and jumping sports.
In the current article (click here for the abstract) Meyer, Brent, Ford and Hewett unveil a new screening tool involving the tuck jump. They propose that this tool is easier for the S & C coaches to do on the field and not only assess risk factors by way of observing technical flaws, but also use the tool as a training maneuver.
The idea is the subject will perform tuck jumps for 10 seconds consecutively while the observer makes notes on the following pre, mid and post jumping:
- Lower extremity valgus at landing
- Thighs do not reach parallel (peak height of jump)
- Thighs not equal side-to-side (during flight)
- Foot placement not shoulder width apart
- Foot placement not parallel (front to back)
- Foot contact timing not equal
- Excessive landing contact noise
- Pause b/w jumps
- Technique declines prior to 10 seconds
- Does not land in same footprint (excessive in flight motion)
Factors 1-3 refer to knee and thigh motion, 4-7 refer to foot position during landing and 8-10 refer to plyometric technique. Coaches are instructed to grade the flaws if seen with check marks during the phases they are seen and use this as a guide for correction. They may also use cameras in the frontal and sagittal plane to assist them.
My thoughts on this are:
- There is sound science behind the rationale for the test and modifiable risk factors
- There is a need for basic no-cost screening tools coaches can apply in their settings
- The tuck jump assessment will provide instant feedback on form and identify technical flaws that may indicate higher risk for injury
- The tuck jump is a higher demand plyo drill so I fear poor form may be as much to blame on inexperience and unrefined motor patterns as it is to just dominance patterns so we need to keep plyo training experience in mind when analyzing the screen results especially for beginners
- The tuck jump assessment does not really consider fundamental movement restrictions that may bias the form on one side if an asymmetry is present
- I still wonder how much ankle pronation impacts landing and whether we will see more research on this – there was a study done at ECU where they used orthotics and saw a reduction in ACL tears in their collegiate athletes so I have to wonder about this crucial element of the kinetic chain
In the end, we still lack many answers. According to data published in the Journal of Athletic Training in 2006, non targeted neuromuscular training programs need to be applied to 89 female athletes to prevent 1 ACL tear. So, we need to keep studying and applying science to our training, all the while critically questioning science and looking at our athletes holistically to find the best prevention strategies for each one individually and for at risk athletes as a whole.
I have been attending the 26th Annual Cincinnati Sports Medicine Advances on the Shoulder and Knee conference in Hilton Head, SC. This is my first time here and the course has not disappointed. I have always known that Dr. Frank Noyes is a very skilled surgeon and has a great group in Cincinnati as I am originally an Ohio guy too.
So, I thought I would just share a few little nuggets that I have taken away from the first three days of the course so far. I am not going into great depth, but suffice it to say these pearls shed some light on some controversial and difficult problems we see in sports medicine.
Shoulder Tidbits
- Fixing SLAP tears may not always fix shoulder pain as in many cases it may be in part due to posterior capsule tightness and anterior instability leading to internal impingement. Additionally, many of the docs here choose not to repair type 2 tears in those over 40 tears and provide a biceps tenotomy or tenodesis to instead to deliver more predictable pain relief as opposed to a labral repair.
- Intraoperative pain pumps in the shoulder are causing glenohumeral joint chondrolysis in the shoulder in many cases. According to the panel of docs, this has been seen in teenagers and patients in their twenties as well. They have often undergone other procedures from outside docs and then developed increasing pain afterward. Many have had to even undergo a total shoulder replacement after a few years post-op. The MDs here have suggested even post-operative Marcaine injections for pain relief in the shoulder should probably not be used. It was very sad to see an 18 y/o shoulder x-ray they put up that looked as if the patient was 80 years old.
- Double row rotator cuff tendon repairs seem to outperform single row repairs with respect to tendon healing (90% for DR and 76% for SR techniques in a comprehensive review of the literature)
- Stretching cross body horizontal adduction may be more important for throwers and overhead athletes than the sleeper stretch – best to have a therapist stabilize the scapula and then move the shoulder across the body keeping the shoulder in neutral rotation (it will tend to externally rotate)
- Arthroscopic stabilization is better than open surgery for posterior shoulder instability as the posterior cuff and deltoid are not violated, ROM recovery is more predictable, patient satisfaction is higher and there is a more predictable return to sport
Knee Tidbits
- Increased femoral anteversion and torsion is a developmental factor that does in fact control the knee to a great extent. The tibial tubercle-sulcus angle, thigh-foot angle and foot alignment is also key according to Dr. Lonnie Paulos. In cases of miserable patella mal-alignment, many will need de-rotation and re-alignment procedures to improve their symptoms.
- The consensus among the orthopods here was that using a bone-tendon-bone patella tendon autograft to reconstruct torn ACLs in the younger more active athletes (soccer players and football players) is preferable to a hamstring graft or allograft. Allografts did not seem to be the graft of choice by any of the docs for the younger patients. Some would use a hamstring autograft provided there was no MCL pathology. The PTG autograft was the gold standard for years (always my favorite graft choice for high level/demand athletes) so I was pleased to see the trend for this population moving away from the ST/gracilis HS grafts.
- Kevin Wilk, DPT (primary PT for Dr. James Andrews), was advocating restoring full and symmetrical ROM after ACL surgery. I tend to agree with this principle myself. However, Dr. Noyes was not in agreement and rather cautiously noted he would be okay with about 3 degrees of hyperextension on the repaired side no matter how much hyperextension was available on the other side. Kevin also noted that restoring full flexion was paramount to restoring running mechanics and speed in higher level athletes.
- The golden time to repair a MCL tear is in the first 7-10 days. Dr. Paulos also suggested it is absolutely necessary to fix the deep layer as well as the superficial layer. His talk emphasized how big of a mistake it is to not repair the deep layer. He also warns that the strength of the repair is less important than restoring proper length, tension and collagen.
- For PCL augmented repairs, a 2 bundle repair is repaired. Most of the docs like to use a quad tendon autograft from the contralateral thigh, but will take it from the same leg if patients insist. The consensus seemed to be that a repair should be done if there is 10 millimeters or more of drop off.
These are just some of the highlights I wanted to pass along. There was lots of other good stuff (much of it a nice review of anatomy, biomechanics and protocol guidelines for rehab) but I wanted to pass along some of these key items while they were fresh in my head. I will likely be sharing more in the future, particularly with respect to patello-femoral pain and SLAP tears as these are just so controversial in terms of surgical and rehab management.
The News and Observer (our local paper here in the Triangle) recently ran a great story on overuse injuries in young athletes. I firmly believe this is one of the fastest growing injuries I see in the clinic and in many cases it is preventable. One of the biggest issues now is this commonplace idea that gifted athletes should play the same sport year-round to get ahead.
I remember growing up as a kid and playing football, basketball and baseball in the fall, winter and spring. While AAU basketball and Legion ball existed, most kids were still playing multiple sports. Over my 15 years as a physical therapist I have witnessed several of these one sport stars see their playing time and bodies take a hit due to injury.
The American Orthopedic Society for Sports Medicine (AOSSM) and the American Academy of Orthopedic Surgeons (AAOS) state that overuse injuries account for nearly half of the 2 million injuries seen among high school athletes each year. While soccer and swimming seem to send many athletes into PT, any repetitive throwing or overhead activity bears considerable risk for an eventual shoulder or elbow problem as well. Some of the common injuries I typically see are:
- Patellofemoral pain
- Shin splints
- Rotator cuff injury
- Bursitis
- Shoulder instability
- Little League elbow

Little League Elbow (medial epicondylar apophysitis)
These injuries are just some of the most common ones I see. In the article, the reporter focused on baseball and throwing. With that in mind, consider research published in the American Journal of Sports Medicine this past February from renowned surgeon James Andrews that revealed players who pitch more than 100 innings in a calendar year are 3.5 times more likely to be injured.
He goes on to say that “these injuries are the result of a system that prepares genetically gifted athletes to play at the highest levels, but eliminates most players because their bodies cannot withstand such intense activity at such an early age.” Sadly, he told the reporter that in 1998 he performed the Tommy John procedure on 5 kids high school age or younger, while in 2008 he did the same procedure on 28 children in the same age range. This injury is usually caused by throwing too much too soon.
Consider the following data on suggested pitch counts per game (source James Andrews, MD & Glenn Fleisig, MD):
- 8-10 y/o = 52 plus/minus 15 pitches
- 11-12 y/o = 68 plus/minus 18
- 13-14 y/o = 76 plus/minus 16
- 15-16 y/o = 91 plus/minus 16
- 17-18 y/o = 106 plus/minus 16
Unfortunately, I can personally relate to this blog post and story. I was a promising young pitcher up until the point I threw my arm out in travel baseball at age 13. The pain got so bad in my arm I could barely throw a ball 10 feet. I remember the orthopedic surgeon telling me that I could not throw again the rest of the summer. The pain (and memory of it) was so bad I elected to focus on position play and not to pitch again until my senior year of high school. At that point, my arm was no longer the same as I had missed three years of practice and development. Now, I too had become one of those kids whose body was never the same.
So, as a rehab and strength & conditioning professional, I want to help educate and promote better awareness to athletes, parents, coaches, trainers, AD’s, ATC’s and anyone who is involved in the care and training of young athletes. Fortunately, people are taking positive steps to reduce overuse injuries. One great initiative is STOP – Sports Trauma Overuse Prevention and you can learn more by clicking here to visit their website.
In the end, we must continue to educate everyone that the old motto of “No Pain, No Gain” is NOT the way to handle overuse injuries as this mentality may ruin the careers of young athletes or lead to an otherwise preventable injury and/or premature musculo-skeletal damage. Pain truly is a warning signal the body gives us to detect mechanical problems and make changes in our training/activity level until we sort out the cause and solution. I hope you will join me in supporting this mission and working hard at making sports fun, safe and free of overuse injuries for young athletes of all ages in the years to come.
References – The News & Observer – May 15, 2011

