Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
As I prepare to present at an ACL Symposium with some of my colleagues this weekend, I thought I would share some of the information I am presenting on injury prevention.
Research consistently shows that neuromuscular training is beneficial in reducing ACL injuries. This type of training hinges on training our athletes to land, plant and cut on a bent knee while shifting the COM (center of mass) forward. Too many times, I see female athletes land with stiff knees in an upright posture relying too heavily on their quads.
Emphasizing hip and knee flexion is vital in order to activate the posterior chain and provided a restraint to anterior tibial translation. When it comes to landing and plyometrics, I feel strongly that we need to focus on repetitive drills that enhance power and teach ideal form.
These exercises should include single and double leg varieties, but more importantly they should challenge the body in the sagittal, coronal and transverse plane. I have included a short video today that illustrates just a few exercises that I incorporate in my training sessions.
Stay tuned as I will share more details about prevention training in future posts.
First off, I want to extend warm Holiday wishes to all of you reading this blog!! As I sit at home on Christmas Eve morning, I am quietly reflecting back on a big year of accomplishments and changes I experienced in 2010. It is often hard to take time to appreciate your blessings, Because as a society we are driven to conquer the “next thing.” However, I have been trying to get better at taking time to savor life’s victories.
Last year, I ran my first marathon (thankfully under 4 hours despite horrible cramps), sold my successful 10 year-old fitness business in Ohio, and moved to North Carolina to tackle a new venture at the Athletic Performance Center. The past year has truly been full of many changes and blessings.
Over the years, I have come to realize that the real gift in my profession is being able to help others. For me, I have an ability to reach consumers through my rehab and performance training, as well as my peers through blogging, speaking and products. If you read my blog, I hope that I have been able to help you even if it is only in the smallest way.
As I look ahead to 2011, I am excited for new opportunities and feel like it will be a big year of learning and exploration for me. That will translate into more sharing on this blog and in my monthly Training & Sports Medicine Update Newsletter. I am continuing to write for PFP Magazine through my online column and will share my latest post with you today on crossing lunges.
Performing a crossing lunge presents unique challenges to the body – challenges which often exploit muscle imbalances, mobility issues, and balance deficits. It is a rotational activity that is more challenging then it may appear.
I once had an athletic trainer question the safety of them in an exercise class I was teaching. She thought they were harmful for the meniscus in the knee. Hmmm…. If that is true , why would I do them? Well, like any exercise you do in the gym, there is always risk of an injury IF you do the exercise improperly. That is a key takeaway point. For the record, I never recommend an exercise I think is dangerous – in most cases it simply comes down to form and knowing your limitations.
Crossing lunges are very effective in strengthening the entire lower body, but particularly the hips. Whether choosing the backward or forward variation, they call for hip internal/external rotation, knee stability and ankle mobility. Beyond that, they are very functional for sport and athletic movement.
Think about field or court sports for a minute. How many times does an athlete cross over to dribble, scoop up a ball or evade a tackle? You may see the forward variation more, but the backward variation is seen as well with drop steps, pivot motions and even along the baseline in tennis.
So, if you train athletes or are an athlete, this is a great example to keep in your personal exercise tool box. I have included pictures of the forward and backward version below. See the link below the photos for my full column and explanation of how to do the exercise properly.

Backward Crossing Lunge (onto right)

Forward Crossing Lunge (onto right)
Click here to read my full online column, Functionally Fit, pertaining to this lunging exercise. Thanks for reading this, and I wish you all the best in the year to come!
Whenever I speak at fitness industry events, I always tell my fellow fitness comrades that they must do everything in their power to elevate the profession. I live in both the “rehab” and “training” world daily. I can tell you unequivocally that the words “personal trainer” do not garner tons of respect in the medical community in many cases.
I will share a personal story from my professional work experience this week that illustrates why. Yesterday, I evaluated a new patient (45 y/o male) who just underwent an ACL allograft reconstruction and medial meniscectomy for a medial meniscus tear. See the image below for an illustration of an ACL tear.

When I asked the patient how his injury occurred he replied, “I tore my ACL doing a plyometric workout with the personal trainer at my work.” Ouch! Naturally I wanted to know more. So, I pressed him for more information – things like:
- What kind of plyometrics
- How many
- Were they at the beginning or end of the session
- How long had you been doing them
Let me tell you that a lot of therapists would not have asked these questions. They would have moved on in the evaluation, dismissing this trainer as an incompetent fitness pro in their mind. The fact of the matter is that bad things do happen at times even when we are doping everything just right so I like to give people the benefit of the doubt in most cases.
However, some of his answers led me to believe this particular trainer needed further education. My client said the entire 30-40 minute workout was plyometrics. He was doing single leg multi-directional hops, but actually tore the ACL during a broad jump. He mentioned he had only done a handful of the workouts before getting injured. The kicker was when I asked him if anyone else in the class had been injured, and he remarked that another man recently tore his Achilles tendon.
For those who know me well, it is safe to say I am an “ACL geek” of sorts. I love studying, reading and searching for the best way to rehab and prevent these injuries. As I have grown in the profession, I have become increasingly concerned with articular cartilage damage and the long term effects it has on our young athletes.
Perhaps I am getting more concerned as my knees aren’t getting any younger either (lol). Anyway, I truly believe we often underestimate how deleterious cartilage injuries can be long term. In addition, I feel we, as rehab and conditioning professionals, need to better understand how our training impacts the cartilage regardless of whether patients had a concomitant bone bruise with their ACL injury or not.
One of my favorite prehab exercises is a single leg hop and stick (see below)

I typically begin with an alternate leg approach (push off right and land on left) prior to initiating takeoff and landing on the same leg to teach proper landing mechanics. By now, we know increasing hip and knee flexion, as well as shifting center of mass forward reduces ACL strain and injury risk through a diminished extension moment.
However, what we may not know as much about is how an ACL reconstruction alters tibiofemoral joint mechanics at such a landing. I want to share some interesting information from a recent article in the September edition of The American Journal of Sports Medicine. The article by Deneweth et al. looked at tibiofemoral joint kinematics of the ACL reconstructed knee during a single-legged hop landing.
So, I have been swamped with work and marathon training, hence the recent delay in a new blog post. Well, yesterday during a short 3 mile run (I am in taper mode with a 10/17 event) I experienced an acute left hamstring strain.
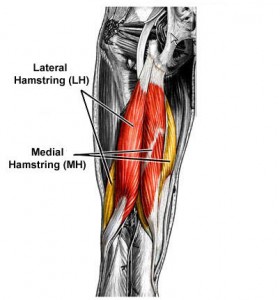
Hamstring strains are common and can produce incredible pain and limit function. Most hamstring strains occur as the swing leg is coming forward and the knee is nearing full extension. Essentially, it is a stretch type injury as the hamstring works to decelerate the momentum of the lower leg.
Injuries may be casued by inadequate warm-up, a sudden increase i training intensity/volume, fatigue, stiffness, weakness or muscle imbalances. A prior injury may also increase your risk for re-injury.
I have been running for years and am 5 months into my marathon training, so why now? I honestly think it may be related to my speed yesterday. My body naturally leans toward a 7:25 pace, but when I looked down at my Garmin yesterday at the point of pain, it said 6:54. Yikes! I was 1.25 miles into the short run.
I decided to keep running and slow my pace back to 7:30. While I was able to complete the run, my lower hamstring was very tight and sore after the run. Obviously, I have been icing regularly the last 24 hours. No running today either. I anticipate a quick recovery since the strain is mild and I am very fit. But, what is the best way to prevent re-injury?
I have a quick article summary from the Journal of Sports & Orthopedic Physical therapy Journal for you to read that underscores how important functional movement rehab is in comparison to just static stretching and strengthening.
Click here to read the summary of the journal article
Now, with respect to running, agility may not be necessary. Running is fairly linear (straight line) so what may be more important to gage capacity to return to running may be some of the following:
- Absence of pain with active knee straightening
- Absence of pain with walking
- No pain with single leg hopping
- Minimal to no muscle belly tenderness
In the end, you will need to let pain guide you. Some will return faster than others, but inside of 21 days (the end of the subacute healing phase) you must be aware of the fragility of the tissue as it heals. I am confident this will not derail my marathon, but the lesson learned is to watch your starting pace as it may lead to some muscle strain.

