Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
This post is dedicated to improving mobility in two areas I commonly find restrictions in among my clients – the ankle and thoracic spine. Specifically, I often find limitations in dorsiflexion and thoracic spine rotation that create undue stress on other parts of the kinetic chain.

Standing wall touch
Recently, I wrote an article for the WeckMethod site on how to assess and improve ankle mobility. As a clinician and coach, I see this issue in many runners and athletes I work with. At times, it is joint restriction, while in other cases it is soft tissue limitations that impact mobility.
There are several potential reasons why one might possess less than optimal movement in the ankle. The most common causes include: joint stiffness following injury and/or immobilization, soft tissue tightness in the gastroc/soleus complex, scar tissue from a prior injury, anterior ankle impingement, chronic ankle instability and adaptive shortening of the Achilles tendon. Want to read more?
Click here to read my article on the WeckMethod site
Decreased mobility in the thoracic spine often creates dysfunction and stress on other parts of the kinetic chain, namely the shoulder and lumbar spine. In many cases, clients will demonstrate asymmetry based on their sport, activity level and injury history. In light of this, I often prescribe a simple, yet effective corrective exercise they can do at home to restore motion. The exercise below is taken from my ‘Functionally Fit’ column I recently did for PFP Magazine.

Side lying t-spine roll
In the full online column, I reveal two ways to do this and the applications for it. This exercise also offers a way to assess your own range of motion, while teaching you a straightforward corrective exercise to improve mobility.
Increasing shoulder, torso and hip strength and stability is a common training goal for athletes involved in sport. Facilitating hip disassociation and kinetic chain linking with exercise is always a plus. I like to use a diagonal mountain climber with hip extension to accomplish these objectives. More specifically, I utilize this exercise with my overhead athletes and anyone involved in cutting, pivoting and rotational sports.
Begin in a tall plank position. The hands should be beneath the shoulders with the feet on the floor and shoulder width apart. Slowly bring the left knee/hip under the body and toward the right elbow. Pause at the end point prior to losing form or control.
Next, return the left leg toward the start position and up into full hip extension in one continuous movement. Pause at the top end of available hip extension and repeat the cycle for 10 repetitions or time on the same leg. Alternate legs and perform 2-3 sets on each side.
Sufficient upper body strength and core/hip stability in a 3 point position is necessary to perform the exercise correctly. At no time should the foot of the moving leg touch the floor or be used to balance the body. As far as a pace, I feel using a 1/1/1/1 cadence works best.
This exercise is an excellent way to promote shoulder, core and hip stability while facilitating hip disassociation as well. Driving the hip back up into extension will activate the gluteals and simultaneously force the stable (fixed) hip to stabilize the pelvis and counterbalance the movement pattern. In addition, the client will have to effectively activate the hip and abdominal musculature throughout to avoid unwanted pelvic tilt/rotation during the movement.
Click here to view the full video of this exercise I did for my ‘Functionally Fit’ column for PFP Magazine.
Baseball pitchers who fail nonoperative care for SLAP injuries will undergo a repair if they wish to continue throwing. The injury may occur at ball release as the biceps contracts to resist glenohumeral joint distraction and decelerate elbow extension. The other thought is that injury occurs in late cocking as the result of a “peel back” mechanism when the abducted shoulder externally rotates. Previous research by Shepard et al. published in American Journal of Sports Medicine (AJSM) measured in vitro strength of the biceps-labral complex during the peel back and distal force and concluded that repetitive force in both scenarios likely causes SLAP lesions.

“Baseball pitching motion 2004“. Licensed under CC BY-SA 3.0 via Wikimedia Commons.
One of the concerns for pitchers after surgery is regaining full shoulder external rotation and horizontal abduction. If too much tension is placed on the glenohumeral ligaments during surgery, regaining motion can be tough. Ironically, external rotation is limited in the early phase of rehab to protect the labral repair which may impair throwing mechanics later on. Appropriate rehab and progression is paramount for long term success.
Laughlin et al. at the ASMI sought out to explore in a labaratory if there are differences in pitchers who underwent a SLAP repair compared to those in age controlled groups without injury. In a paper published in the Dec. 2014 AJSM, the researchers hypothesized that the SLAP group would exhibit compromised shoulder range of motion and internal range of motion torque during pitching. Of 634 pitchers (collegiate and professional) tested at ASMI from 2000 – 2014, 13 in this group were included in the SLAP group as they had undergone a SLAP repair at least 1 year before their biomechanical testing.

I hope you and your families had a wonderful Thanksgiving holiday! Starting today and running all week you can save 30% on any and all of my DVDs. Take advantage of this offer on any of my Fit Knee series (osteoarthritis, running, or ACL) as well as my Ultimate Rotator Cuff Training one. The sale will end on Sunday Dec. 7.
Please share this offer with friends, colleagues and family who may benefit from any of these products. Simply enter code DVD30 at the checkout and hit apply coupon to save 30% today. Click here to order.
I see plenty of pitchers in my clinic ranging from 12 y/o travel baseball players to MLB guys. My own son is a left handed pitcher so I am always carefully watching his mechanics, pitch count and arm care. There has been much written about glenohumeral internal rotation deficit (GIRD) and total shoulder motion over the years.
Today, I wanted to recap a nice article that was recently published in the American Journal of Sports Medicine by Wilk et al. looking at deficits in glenohumeral passive range of motion (PROM) and the increase in elbow injury risk.
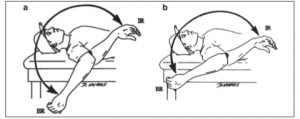
This prospective study was done over an 8 year period from 2005-2102 and looked at PROM of both throwing and nonthrowing shoulders of all major and minor league pitchers within a single baseball organization. The measurements were taken with a bubble goniometer during spring training. See images below from the journal article for how measurements were taken:

In sum, 505 exams were performed on 296 pitchers. Motion was assessed in supine with the arm abducted to 90 degrees and the arm in the plane of the scapula. One examiner stabilized the scapula, while another measured total rotation and passive flexion. Elbow injuries and days missed because of injuries were assessed and recorded by medical staff. Throwing and nonthrowing measurements were compared, while additional testing was done to find significant associations between shoulder motion and elbow injury, as well as odds of an elbow injury.




