Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
I have a steady flow of baseball players who come to see me for shoulder and elbow rehab. As a former pitcher whose playing career was altered by an arm injury at age 14, I have a particular interest in throwing injuries. My son is a 6’2″ left-handed pitcher that plays showcase baseball. He will be the subject matter of this post moving forward.
Many of the players I see for shoulder and elbow pain suffer from pathological GIRD (glenohumeral internal rotation deficit). While it is common to see throwers with less internal rotation on their dominant side, it is important to assess total shoulder motion to make sure their mobility is within 5 degrees of their non-dominant side. Asymmetry in total shoulder motion and shoulder flexion increase the odds of elbow injuries. Click here to see the correlation in professional pitchers. Additionally, insufficient external rotation gain on the throwing arm increases injury risk. Click here to read an abstract summarizing data within the same group of professional pitchers.
Given this information and my background, I have preached arm care for years to my son. For some background, my son has pitched since he was 9 years old. Since I have been a coach for his team in one capacity or another since he was 10, I have closely monitored and controlled his pitch counts, innings per outing and total innings per year. He has always been able to throw hard, but he had a big growth spurt in middle school and his velocity grew with that.
He now throws between 75-77 mph as a HS freshman. He is projected to be 6’5″ tall and weighs 170 pounds at this time. His showcase coach pitched in MLB, and we have two other organizational pitching instructors with big league experience who supervise his weekly bullpens. His total innings pitched for 2017 = 43. Research indicates anything over 100 significantly increases injury risk. With all that said, he has developed some medial elbow pain over the past 4 months. He has no history of arm trouble to date. My intention is for this post to serve as useful diagnostic and proactive intervention for those who may see and experience similar cases.
Spring training has begun, and youth baseball players all over the country are starting to practice and prepare for their upcoming seasons. My very own 14 y/o son has started his 8th grade season, while having been working with his travel team on the weekends since mid December.
As a physical therapist, former player, father, and assistant coach on his 14U team, my first concern is always the health of a player. I see several baseball players in my sports medicine practice ranging in age from 9 year olds to MLB platers. Diagnoses include internal impingement, SLAP tears, little league elbow/shoulder, OCD, UCL sprains, rotator cuff tendinitis, instability, fractures and scapular dyskinesia.
One of the hardest things to do in my profession is get inside the head of a young athlete. Many will refrain from mentioning pain for fear of letting down a parent or coach, or out of concern for losing playing time. Society has become too focused on early specialization and winning from an early age. In addition, “travel baseball” has been somewhat diluted and water down by lots of dads who want their sons to play year-round. I often see kids being abused on terms of too little rest or improper recovery after they pitch and catch.
The biggest, most athletic and hardest throwing kids undergo the most strain as they are asked to shoulder the load at pitcher, catcher and shortstop early on. Many coaches are counting innings in tourneys and not pitches based on tournament guidelines. Too many kids are pitching on consecutive days without proper rest all in an attempt to win meaning less tournaments at a young age. Fortunately, we are making progress in the sports medicine world thanks to the efforts of Dr. James Andrews and others.
High schools are adopting pitch count regulations this year, and MLB along with Dr. Andrews has developed their site, www.pitchsmart.org, to spread education about injury prevention in youth pitchers. Dr. Christopher Ahmad is on the advisory committee for PitchSmart.org, and he is also the lead author on a new paper detailing an injury assessment tool for young baseball players, The Youth Throwing Score.
It is no secret that elbow injuries have been on the rise in MLB as well as all levels of baseball. I see far too many adolescent baseball pitchers in my clinic with medial elbow pain. Often it is related to pathological GIRD and proximal imbalances in the shoulder complex.
Researchers have been studying biomechanics for years. It has long been a belief that younger pitchers should focus on fastballs and change-ups, while minimizing curveballs. Currently, the prevailing thought and latest evidence seems to suggest that velocity may be the bigger risk factor or determining factor in leading to UCL injuries.
A paper in the August 2016 edition of the American Journal of Sports Medicine from Rush University Medical Center sought to determine factors associated UCLR among MLB pitchers. The hypothesis was that those pitchers who underwent UCLR would have a higher pre injury pitch velocity.
This retrospective case controlled study looked at data for pitch velocity, type and number for every pitcher and game were gathered from the PitchFx database from April 2, 2007 to April 15, 2015. Data from 2013 – 2015 was excluded to avoid lead in time bias, as pitches in these seasons may contribute to injuries in pitchers who have not yet undergone UCLR. Pitchers were classified as control, pre injury or postoperative.

So, I just returned from the Combined Sections Meeting for the APTA that was held in Indianapolis. There was lots of great networking and presentations to be sure. I attended sessions on ACL rehab/prevention, femoroacetabular impingement, elbow injuries in throwers, running gait analysis, and shoulder plyometric training with the legendary George Davies. I thought I would give you my top 10 list of helpful nuggets I picked up over the weekend in no particular order of importance.
1. Performing upper body plyometrics has no effect on untrained subjects so don’t waste time putting it into the rehab program, where as it does benefit trained overhead athletes. The one caveat is it also increases passive horizontal external rotation so keep this in mind when working with athletes who have shoulder instability.
2. A new study coming out in 2015 in AJSM revealed no major differences in throwing kinematics between those following UCL reconstruction (Tommy John) and age-matched controls. This is good news for those worried about pitching mechanics after the procedure.
3. According to Dr. Reiman at Duke, the orthopedic hip exam does a better job of telling us they do not have a labral tear than it does telling us they do have an intra-articular problem. The tests have poor specificity. In fact, he goes on to say that the “special tests are not that special.” That brought a chuckle from the crowd including me. Bottom line – we are not really able to conclusively say “yes you have a labral tear based on my exam today.
4. Reiman also feels we must consider look for mechanical symptoms during the lowering portion of the Thomas test, while considering the fact that fat pad impingement may cause anterior hip pain as opposed to joint pain. Again, things are not always as they appear in the “FAI” crowd so we need to take a great history, look at the classic tests and also see how squatting and loading affects the hip.
5. More experienced pitchers do not drop the glove side arm, but instead tend to move their body toward the glove to conserve angular momentum and overcome small moments of inertia. Less experienced pitchers rotate their trunk sooner in pitching cycles whereas pitchers who threw at higher levels rotated later and produced less torque at the shoulder. Consequently, many players with higher elbow valgus torque and distraction force at the shoulder rotate too early.
I see plenty of pitchers in my clinic ranging from 12 y/o travel baseball players to MLB guys. My own son is a left handed pitcher so I am always carefully watching his mechanics, pitch count and arm care. There has been much written about glenohumeral internal rotation deficit (GIRD) and total shoulder motion over the years.
Today, I wanted to recap a nice article that was recently published in the American Journal of Sports Medicine by Wilk et al. looking at deficits in glenohumeral passive range of motion (PROM) and the increase in elbow injury risk.
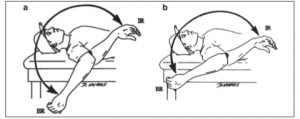
This prospective study was done over an 8 year period from 2005-2102 and looked at PROM of both throwing and nonthrowing shoulders of all major and minor league pitchers within a single baseball organization. The measurements were taken with a bubble goniometer during spring training. See images below from the journal article for how measurements were taken:

In sum, 505 exams were performed on 296 pitchers. Motion was assessed in supine with the arm abducted to 90 degrees and the arm in the plane of the scapula. One examiner stabilized the scapula, while another measured total rotation and passive flexion. Elbow injuries and days missed because of injuries were assessed and recorded by medical staff. Throwing and nonthrowing measurements were compared, while additional testing was done to find significant associations between shoulder motion and elbow injury, as well as odds of an elbow injury.




