Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
I work with lots of patients and clients who consistently demonstrate inadequate hip and core stability. I see this show up routinely as asymmetrical 1’s for the trunk stability push-up, in-line lunge, hurdle step and rotary stability movements on the FMS. Unfortunately, this has been a recurring them in many of my females recovering from ACL reconstruction as well as runners with persistent pain/dysfunction in one lower extremity.
I am always looking for better ways to train the body in whole movement patterns as well as functional positions. One of my preferred positions is to test and challenge my clients in a split squat position. I begin with an isometric split squat cueing proper alignment and muscle activation. As clients master isometric postural control, I will allow them to add an isotonic movement by squatting in the position.
As they progress, I will add in perturbations to stimulate changes or challenges to their center of gravity. Often, you will see them struggle much more on the involved side. But to be honest, I find most people have an incredibly hard time maintaining proper alignment for long without cheating or falling forward or to the side. Allowing clients to lose form is okay provided they are cued to fix their alignment or they naturally self correct.
An additional wrinkle I throw in for this training is using the BOSU Balance Trainer. Below is a video that shows how I use this progressing from shin down to just the toes as a support on the trail leg. The second version will burn up your clients’ thighs and quickly become one of their least favorite exercises. The great thing is that you do not have to offer much resistance to create a significant perturbation.
For more detail on this exercise and application, click here to read my PFP column featuring it this week.
While I treat a vast number of knee ailments in my practice, the focus of my training and rehab is often more proximally directed at the hip. Understanding the role of hip muscles and how the hips and pelvis work together to impact knee alignment and closed chain function is critical in resolving knee pain and dysfunction.
Below is a “go to exercise” exercise I use for gluteus medius activation and core/pelvic stability training. Using a mini-band provides an adduction force cueing the client to abduct and activate their external rotators to maintain proper alignment. Additionally, they need to avoid a drop on one side of the pelvis (look at the ASIS).
Click here to read my entire column dedicated to this exercise in PFP’s online magazine. I hope you find this exercise and information useful for you and/or your clients.
Research along with years of observation has taught me that the brain is inherently looking for the most efficient way (aka least effort) to execute movement in life. In addition, it HATES pain just like you and I so it does everything possible to avoid it including ordering the body to perform dysfunctional movement patterns.
After a painful episode, the brain often needs reminded that the body can go back to the proper movement patterns once the pain is gone. However, it often holds that painful memory and may by default lean toward a faulty movement pattern. This protective mode then ends up perpetuating a faulty movement pattern that is no longer necessary nor efficient. Over time, dysfunctional movement patterns can create further stress or harm to other segments in the kinetic chain.
So, I am always seeking ways to stimulate the body to work properly and exercises that facilitate proper neuromuscular patterning are instrumental in my rehab and training. I wanted to share two exercises that I like to utilize in my rehab and training for the shoulder. In particular, I like to employ closed chain activity to stimulate the serratus anterior as well as the other scapular stabilizers.
Below are two exercises I wrote about in my “Functionally Fit” column for PFP magazine. The first exercise shows quadruped rocking. Shirley Sahrmann mentions this in her work, Diagnosis and Treatment of Movement Impairment Syndromes. I began using it after reading her book, and I agree that it works very well for scapular dysfunction. Below is the start and finish position for the quadruped version as well as my own advanced tripod version of the exercise.
- Quadruped start
- Quadruped finish
- Tripod finish
For a complete explanation of the exercise and its application, click here to read the column.
As a follow-up to this exercise, I included an unstable progression I like to employ using the BOSU trainer. I call this the unstable tripod scapular clock. It can be done on the knees or up on the toes. I have included a quick video on this below. Again, I like this exercise for scapular work as well as core stability training.
Click here to read my PFP column on this exercise for the full description, application and regressions. The real beauty of this last exercise is the “big bang for your buck” attributes since it hits shoulder, core and hip stability all at once for those able to work at that level. I hope it works as well for you as it has for me!
There seems to be consistent questions, debate and studies done with respect to stretching. As the thought of more closely analyzing the quality of movement (FMS, Y-Balance testing, SFMA for example) moves to the forefront in the PT and fitness world, many search for the right mix of exercise to maximize mobility.
I count myself as a supporter and follower of the work of Gray Cook and Stuart McGill. While I may not agree 100% with all of their ideas, I generally consider them to be brilliant minds and ahead of the curve. I have been using the FMS in my practice for some time now and have also begun to incorporate Y-Balance testing as well (see pic below courtesy of the IJSPT)
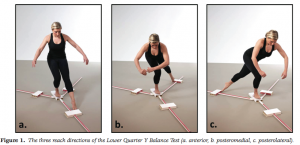
The Y-Balance test may not have significant relevance to hip mobility as much as it does limb symmetry, but I included it here to illustrate my point in observing kinetic chain movement to help determine where the weak link or faulty movement pattern may be. It gives us valuable information with respect to strength, balance and mobility.
With the revelation that FAI is more prevalent than we knew (click here for my post on FAI), I am always interested in hip mobility and how to increase movement in the hip joint. Limitations in hip mobility can spell serious trouble for the lumbosacral region as well as the knee.
I currently use foam rolling, manual techniques, dynamic warm-up maneuvers, bodyweight single leg and hip/core disassociation exercises and static stretching to increase hip mobility. However, I am often faced with the question of what works best? Is less more? How can I make the greatest change without adding extra work and unnecessary steps?
Well, Stuart McGill and Janice Moreside just published a study in the May 2012 Journal of Strength & Conditioning Research that sought to examine three different interventions and how they improve hip joint range of motion. Previous work has been focused on the hip joint alone, and they wanted to see how other interventions impacted the mobility of the hip. Click here for the abstract
It is widely accepted that decreased hip strength and stability leads to knee valgus. Excessive frontal plane motion and valgus torque increase the risk for non-contact ACL injuries. While we know that hip abductor weakness is more of an issue in females than males, the question remains to what degree other factors are involved.

Claiborne et al (1) noted that only 22% of knee variability could be linked solely to hip muscles surrounding the hip. In light of this we must look at the whole kinetic chain when assessing movement dysfunction and injury risk. In the most recent issue of the IJSPT, researchers sought to discover how activating the core during a single leg squat would impact the kinematics of 14 female college-age women. They excluded participants with current pain or injury to the lower extremities or torso, or if they had a history of any lower extremity injuries or surgeries in the past 12 months.
The participants were assessed for their capacity to recruit core stabilizer muscles using lower abdominal strength assessment as described by Sahrman (2). This testing model has 5 levels of increasing difficulty used to challenge participants to maintain a neutral spine. The draw back of this method is that it is done in supine versus the standing position of this study, but the author acknowledges this limitation. Out of a possible high score of 5, five of the participants scored a 1 or 2, while the other nine scored a zero.
For the study, a six inch step was used to assess 2 reps of a single leg squat. Each participant was asked to perform the test with the dominant leg to standardize conditions. They performed the reps under two conditions:
1. CORE – engaged abdominal muscles as they had been instructed to do so during the Sahrman test
2. NOCORE – no purposeful engagement of abdominal muscles
Results
- The CORE condition resulted in smaller hip displacements in the frontal plane but had no effect on hip angular range of motion – essentially there was less medial/lateral movement
- The CORE group did not exhibit any changes in knee displacement but did exhibit greater degree of knee flexion – this may suggest higher function assuming more knee flexion is desired during squat tasks in sports and functional activities
- Those scoring the lowest on the core assessments had larger improvements in performance when they did in fact activate the core musculature
How do we use this information to affect our practice? Well, in terms of rehab it seems straightforward and many of us may already encourage patients to activate their core during treatment. However, I think the greater contribution may come in injury prevention programs (particularly ACL programs) where we are looking at all facets of neuromuscular control and appropriate muscle activation patterns.
With any prehab or rehab strategy, we as clinicians, trainers and strength coaches are essentially trying to reprogram the brain to summon and execute a better motor pattern or strategy – feedforward training. We know that healthy individuals tend to have better transverse abdominus and multifidus muscle activation, so it only makes sense to consider activation of local stabilizers as we work on global muscles. Improving core and pelvic stability should only help reduce unwanted frontal plane motion.
With that said, the authors of this study readily acknowledge more work needs to be done with larger clinical populations (including EMG work) to more clearly identify what magnitude the core musculature has on lower extremity motion and displacement.
Keep in mind the proper program will always stem from your ability to assess movement impairment and tissue dysfunction. I suggest beginning with a FMS in the athletic population and incorporating parts of that or the SFMA to compliment your evaluation in the clinic. This will generally reveal the priorities for the corrective exercises. For now, we can use this information in this particular study to be more intentional with our patients and clients suffering knee and hip dysfunction by adding this one simple step to our programming.
References
1. Claiborne TL, Armstrong CW, Gandhi V, Princivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. Journal of applied biomechanics. 2006;22(1):41.
2. Faries MD, Greenwood M. Core training: stabilizing the confusion. Strength & Conditioning Journal. 2007 ;29(2):10.




