Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Well, after a silent stretch the past 2 weeks or so related to my study/preparation for the OCS exam, I am back to blogging! Today’s post is a pertinent one for runners and athletes suffering from lower limb injuries.
Static stretching has taken a bit of a beating in the strength and conditioning world in the last few years. Dynamic warm-ups and active mobility have taken center stage as of late. While these active modalities are certainly superior for prior to practice, play and ballistic activity periods, I still believe stretching has a place in rehab and conditioning.

Interestingly enough, a study recently published in the March 2012 Journal of Strength & Conditioning Research examined the effects of static stretching of the calf and its impact on the strength/ROM of the contralateral side. Click here for the abstract.

In a nutshell, the authors had two groups of untrained individuals: test group (6 male and 7 female subjects) and control group (6 male and 6 female subjects) who participated. The test group did supervised active right calf stretching 3 days per week for 10 weeks (four 30 sec stretches w/30 sec of rest between stretches). They stood on a beam 30 cm above the floor with the left knee slightly bent to offload the left leg as well as placing the hands on the wall while they leaned forward allowing the right heel to drop toward the floor until a max tolerable stretch was felt. The knee was straight throughout on the stretch side.
Control subjects did no stretching at all. All subjects were instructed to maintain their normal physical activity but refrain from any resistance training or stretching during the 10 week investigation. The results:
- 29% increase in 1RM calf raise strength on the right
- 11% increase in 1RM calf raise strength on the left
- significant 8% increase in calf ROM on right
- significant 1% decrease in calf ROM on the left (non stretch side)
- No change in strength or ROM for control group
The authors conclude that the results of this study best apply to rehab settings. For example, they suggest that this procedure may be an effective way to combat the loss of strength in limbs that have been immobilized after injury or surgery simply by stretching the mobile (unaffected) side. They also point out that this may be a way to mitigate strength loss when access to traditional strengthening modalities are not readily available.
Clearly, athletes suffering an acute ankle sprain as well as runners suffering soleus/Achilles/lower limb overuse injuries would benefit from such a strategy. So why does this work? Zhou in earlier work describes a cross training effect due to neural adaptations regulated in the spinal cord.
What does this mean for you and me? Well, as someone who works with many runners I am always looking at eccentric control of the G/S complex as well as effective single leg heel raise strength. The idea that stretching the uninvolved side to strengthen the involved side seems like a no brainer. Clients suffering from tendonitis, plantar fasciitis, stress reactions, sprains and other injuries can use this as an early intervention without stressing the involved side.
More importantly, I like the idea of increasing neural adaptation and ROM in the stretch side through eccentric load as the dissipation of ground reaction forces will be more efficient in a calf that effectively handles eccentric loads through a sufficient range of motion. This study definitely highlights the importance of stretching in novice runners and those with tight gastrocs. I am curious if the bent knee stretch would have had a similar effect primarily on ROM – perhaps they will investigate that further in the future.
As we move more toward mid and forefoot running gait, I believe the fitness of the G/S complex will be even more important than before as stress is transferred away from the knee and more toward the foot/ankle complex. Clearly, we need more studies in trained subjects on unilateral stretching to determine if the same effects and degree of impact will be seen, but this study shows some promise for active static calf stretching in the appropriate populations.
One of the most common PT clients I see is an injured runner. There can be a umber of different reasons or factors involved leading up to a running injury, but I wanted to focus on this idea of gait retraining that is taking place today. With the advent of Born to Run and minimalist footwear, people have begun to question and debate what the best way to run is.
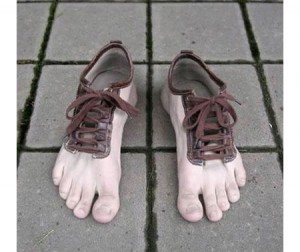
Is this suited for everyone?
Let me just say right away that I do not believe there is a simple answer here. Human beings are all unique and have different genetic and biomechanical makeups. What this means in effect is that they have their own set of “issues” if you will that I classify into common categories such as:
- Static alignment problems (arch, knee, hip, etc)
- Static and dynamic balance deficits
- Inefficient gait mechanics
- Muscle imbalances
- Soft tissue tightness
- Recurring pain patterns
The list could go on and on, but you get the point. The idea of “re-teaching” someone how to run differently than their natural motor pattern dictates in not easy and is a decision that should be well thought out and based on sound decision making. We are pre-programmed at birth with certain native motor patterns and running is one of those patterns. Generally, your brain finds the most efficient way for you to run in your own body.

Now granted, some run much better than others. Perhaps we can say athleticism plays a role in this, but as we grow and reach skeletal maturity our body type, training experience, strength and environment are also major factors . With that said, I know that runners with recurrent and/or chronic pain are looking for a finite solution to their problem. They grow frustrated when they are unable to log all their miles or finish a race.
If traditional PT or relative rest fails to alleviate the pain, we must delve deeper and look more closely at their gait. I think video analysis is a great tool for doing this. We use Dartfish at my clinic, and this is very useful for breaking down gait mechanics and detecting things like heel versus forefoot striking, overpronation, asymmetry side-to-side, trunk inclination, etc. Once we find things on video we must also correlate these findings to our clinical screening to uncover a cause and effect relationship.
I work with many runners in our clinic. I often see restrictions in the soleus. While the running community is warming up to soft tissue mobilization, many runners are still resistant to embrace it routinely and engage in it more so only when they are hurt or lacking flexibility.
STM (soft tissue mobilization) should be part of every runner’s maintenance program. Why? Simply put, repetitive stress takes its toll on the body. Rolling or releasing the tissue increases blood flow, eliminates trigger points, and facilitates optimal soft tissue mobility and range of motion.
In the diagram below, you can see common trigger points in the soleus. The X represents the trigger point & the red shaded area is the referred pain caused by the trigger point.

In the case of the soleus, restricted dorsiflexion could lead to other biomechanical compensations with running. Initially, this often creates a dysfunctional and non-painful (DN) pattern. Over time, this may eventually become a dysfunctional and painful (DP) pattern forcing runners to seek medical care. The terms DN and DP come from Gray Cook’s Selective Functional Movement Assessment (SFMA).
The gait cycle is certainly altered from dysfunction in this muscle. If ankle joint dorsiflexion is compromised (a common effect of soleus restrictions), there can be increased strain on the quads and altered movement in the hip. Overpronation and excessive hip adduction and internal rotation are common compensations seen with running. Other signs and pathology that may be associated with a soleus trigger point may include:
- Plantar fasciitis
- Heel pain
- Shin pain
- Knee or hip pain
- Back pain
As such, restoring mobility is important. A recent study revealed that immediate improvement in ankle motion can be attained with just a single treatment (click here for the abstract).
So how do you effectively resolve soft tissue issues in this area? I suggest using a foam roller or better yet the footballer and baller block in the Ultimate 6 Kit for Runners by Trigger Point (see pic below)

Eliminating the “false step” has been a personal mission of many strength coaches I have heard or worked alongside of in my 15 year career. I used to wonder quietly why it was such a bad thing early on in my coaching. Based on angles and observation it seemed almost reflexive for most athletes.
Then a few years ago I had the privilege of seeing Lee Taft present his theory on speed development and multi-directional speed training and it all came together for me. Lee eloquently explained that the “false step” is really just a plyo step – a chance to load the body up for what it was meant to do. It essentially allows the athlete to reposition the body (or center of mass) more efficiently to load and explode. Ever wonder why sprinters use a starting block?

Look at all like an athlete’s body position once they step back and begin to move forward?
This topic has been covered in previous point/counterpoint articles in the NSCA journals and debated on forums, blogs and seminars alike. For me, I have been encouraging the “false step” or “plyo step” the past few years because it is ‘normal’ for athletes to move that way. As a matter of fact, one of the first things I do is put them in an athletic parallel stance position and ask them to accelerate for 10 yards. Not once have I seen them not step back provided I do not cue them to do so.
Keep in mind that previous research done (Kraan, GA, van Veen, J, Snijders, CJ, and Storm, J. Starting from standing: Why step backwards? J Biomech 34: 211–215, 2001.) indicates that stepping back is instinctive in up to 95% of subjects. Pretty telling, right? Even so, many coaches will still argue this technique slows the athletes down.
One of the greatest things about medicine is that it continues to evolve and change. Sports medicine is at the forefront and athletes are always looking for faster ways to recover and get back in the game. If you are not familiar with platelet rich plasma (PRP) therapy, click here to read my earlier post on it.
It has been used increasingly to treat muscle strains and chronic tendinitis in the heel, knee and elbow. While some early responses have been favorable, there has not been much follow-up data or research available to assess its efficacy. In the August edition of the American Journal of Sports Medicine reports on one-year follow-up for the use of PRP in chronic Achilles tendinopathy.
The study was a double blind randomized placebo-controlled study using 54 patients (age 18-70) who had chronic tendinopathy 2-7 cm proximal to the Achilles tendon insertion (minimum of 2 months). They were randomized and given PRP or a saline injection in addition to an eccentric training program. Keep in mind recent research has indicated the efficacy of eccentric training to treat chronic tendon problems.
In this intervention, patients were given the injection with ultrasonagraphic guidance. After the injection, theyw ere told to avoid sports for 4 weeks. In week 2, they preformed a stretching program. Then all participants began a 12 week eccentric exercise program. Follow-up was done at 6, 12 and 24 weeks by one researcher, while another blinded researcher did the one-year follow-up. Clinical and ultrasonagraphic follow-up was done at each interval.
Results
At the 1 year follow-up, there was no clinical or sonagraphic benefit of PRP. This matches the findings at 6 months as well. One other radnomized studly looking at tennis elbow did find a statistical significance when they compared PRP to a corticosteroid injection at 1 year, instead of a placebo injection. Another key factor or difference is one area is load bearing and the other is not.
In reviewing this study, it should be noted that not only was pain reduction not statistically greater, nor was there any added positive tendon structure changes noted using the PRP. With that said, the looming issue with this treatment intervention is that variables like platelet count, injected volume. number of injections, preactivation and the presence of leukocytes are not always the same across studies, and they were not determined within this study either.
The takeaway here is that there appears to be no added benefit from PRP with chronic Achilles tendinits. However, there is no known negative side effect associated with trying it either. I think the hardest part is scaling back activity and being patient enough to overcome these injuries. In my experience, they often require soft tissue massage, rolling, stretching, eccentric loading, relative rest, and a very specific return-to-activity plan based 100% on the tissue and pain response of the patient.
Time and future research will continue to tell us more about PRP. I think we may find that different growth factors and treatment options may evolve that do in fact speed regeneration and healing.

