Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
One of the most difficult problems to treat in the clinic is chronic pain related to tendinopathy. More specifically, the Achilles tendon, patella tendon and elbow extensors often present challenges for doctors and clinicians alike when it comes to effectively reducing or resolving pain. Over time, people develop chronic inflammation or even little tears in the muscles running up to the lateral epicondyle.

There have been many studies done looking at PRP over the past 5-10 years. The debate continues, however, with respect to its efficacy in terms of results, especially given the fact that patients must currently pay out of pocket for the procedure. I have written two earlier posts on PRP that you may be interested in reading as a back drop for this one:
2011 – An Update on Platelet Rich Plasma
2011 – Platelet Rich Plasma and Rotator Cuff Repairs
Currently, my approach to treating these injuries involves an approach focused on soft tissue mobilization via instrument assisted soft tissue mobilization, stretching, strengthening and a trial of iontophoresis in most cases. We also offer dry needling at our facility and this has been effective in reducing pain. I will talk more about this point later as it relates to the prospective multi-center trial summarized by Mishra et al. in the February 2014 edition of the American Journal of Sports Medicine.
Before I get to the study, I thought it would be pertinent to provide some straightforward information on PRP as it is a question that comes up with patients on a regular basis. Essentially, the process is as follows:
1. Collect 30-60 ml of blood form the patient’s arm
2. Blood is then placed in a centrifuge. The centrifuge spins and separates the platelets from the rest of the blood.
3. A syringe is then used to extract 3-6ml of the platelet-rich plasma
4. The concentrated platelets are then injected into the elbow (or site being treated)

The thought behind PRP is to increase the growth factors up to 8x, which promotes temporary relief and stops inflammation. The question is how successful and cost effective is this process? Consider that opting for surgery will run between $10,000 and $12,000 figuring in costs for the surgeon, hospital/surgery center, anaesthesiologist, etc. PRP injections will cost upwards of $1000, so one would think that would be a favorable option for insurers if surgery could be averted.
What about cortisone injections? They are widely used as a survey of 400 members of the American Academy or Orthopedic Surgeons found that 93% had administered a corticosteroid injection for lateral epicondylar tendinopathy. According to Bisset et al (Br Med J 2006) and Lindhovius et al (J Hand Surg Am 2008) cortisone injections do provide short term pain improvements but also result in a high rate of symptom recurrence. There are other potentially harmful side effects from injections including: reduced collagen synthesis, depletion of human stem cells, depigmentation, and enhancement of fatty and cartilage like tissue changes that can lead to tendon ruptures.
So, the big question is whether or not tendon needling with PRP is an effective treatment option for chronic tennis elbow suffers. Mishra and his colleagues set out to examine this with a double blind, prospective, multi-center randomized controlled trial of 230 patients. In the study, the patients were teated at 12 different facilities over 5 years. All patients had at least 3 months of pain/symptoms and failed conservative treatment.
Rotator cuff tears are common injuries, especially among active middle age men. As researchers and scientists seek for better ways to promote healing and more optimal surgical outcomes, PRP continues to get lots of attention. If you want a basic primer on PRP, click here to read one of my earlier posts on it.
In a recent study in the October 2011 American Journal of Sports Medicine, researchers looked at the effects of PRP on patients undergoing surgery for full thickness rotator cuff tears. This is the first prospective cohort-control study to investigate the effect of PRP gel augmentation during arthroscopic rotator cuff repair. Forty two patients were included in the study (average age of 60), with 19 undergoing arthroscopic repair with PRP and 23 without.
Outcomes were assessed preoperatively and at 3, 6, 12, and finally at a minimum of 16 months after surgery (at an average of 19.7 +/- 1.9 months) with respect to pain, range of motion, strength, and overall satisfaction, and with respect to functional scores as determined using multiple assessment tools. At a minimum of 9 months after surgery, repaired tendon structural integrities were assessed by magnetic resonance imaging.
Below are images defining a full thickness rotator cuff tear:

Partial (left) vs. Full (right)
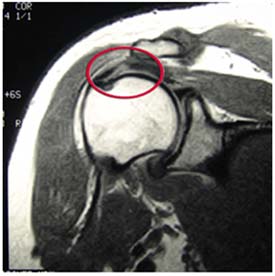
Full Thickness Tear on MRI
One of the greatest things about medicine is that it continues to evolve and change. Sports medicine is at the forefront and athletes are always looking for faster ways to recover and get back in the game. If you are not familiar with platelet rich plasma (PRP) therapy, click here to read my earlier post on it.
It has been used increasingly to treat muscle strains and chronic tendinitis in the heel, knee and elbow. While some early responses have been favorable, there has not been much follow-up data or research available to assess its efficacy. In the August edition of the American Journal of Sports Medicine reports on one-year follow-up for the use of PRP in chronic Achilles tendinopathy.
The study was a double blind randomized placebo-controlled study using 54 patients (age 18-70) who had chronic tendinopathy 2-7 cm proximal to the Achilles tendon insertion (minimum of 2 months). They were randomized and given PRP or a saline injection in addition to an eccentric training program. Keep in mind recent research has indicated the efficacy of eccentric training to treat chronic tendon problems.
In this intervention, patients were given the injection with ultrasonagraphic guidance. After the injection, theyw ere told to avoid sports for 4 weeks. In week 2, they preformed a stretching program. Then all participants began a 12 week eccentric exercise program. Follow-up was done at 6, 12 and 24 weeks by one researcher, while another blinded researcher did the one-year follow-up. Clinical and ultrasonagraphic follow-up was done at each interval.
Results
At the 1 year follow-up, there was no clinical or sonagraphic benefit of PRP. This matches the findings at 6 months as well. One other radnomized studly looking at tennis elbow did find a statistical significance when they compared PRP to a corticosteroid injection at 1 year, instead of a placebo injection. Another key factor or difference is one area is load bearing and the other is not.
In reviewing this study, it should be noted that not only was pain reduction not statistically greater, nor was there any added positive tendon structure changes noted using the PRP. With that said, the looming issue with this treatment intervention is that variables like platelet count, injected volume. number of injections, preactivation and the presence of leukocytes are not always the same across studies, and they were not determined within this study either.
The takeaway here is that there appears to be no added benefit from PRP with chronic Achilles tendinits. However, there is no known negative side effect associated with trying it either. I think the hardest part is scaling back activity and being patient enough to overcome these injuries. In my experience, they often require soft tissue massage, rolling, stretching, eccentric loading, relative rest, and a very specific return-to-activity plan based 100% on the tissue and pain response of the patient.
Time and future research will continue to tell us more about PRP. I think we may find that different growth factors and treatment options may evolve that do in fact speed regeneration and healing.

