Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
For all those following along with my journey, I have moved just past the 8 week post-op mark. I am pleased to report that I continue to see small steady improvements with my mobility during day-to-day activities as long as I am moving below shoulder height. I continue to have periodic and general low-level soreness at times (intermittent) but no marked pain unless really pushing my motion with stretching.
MD Follow-up
I recently saw the surgeon between weeks 6 and 7. He examined the shoulder and determined everything seemed to be progressing fine. I explained to him that I felt my passive range of motion (particularly flexion) felt limited by a pinching pain along the front of the shoulder in PT and at home. I also just felt that the shoulder was more stiff than I had hoped it would be at this point. He recommended giving me a steroid injection to help with inflammation and mobility. He assured me it would in no way compromise the repair.
See the article abstract below regarding early AROM after surgery:
https://pubmed.ncbi.nlm.nih.gov/31084488/
This was my first experience with cortisone. Patients have always told me 1 of 3 things:
- It’s magic and now all the pain is gone
- It hurts more initially but eventually after a few days they noticed some relief
- It did NOT help at all
The response for me was more in line with answer #2. The posterior shoulder was very sore within 2-3 hours after the injection, and the shoulder felt very heavy the rest of the day (motion actually seemed worse). In 24-36 hours, that pain and heaviness subsided, and I would say I could move the shoulder somewhat better in 72 hours. Since the injection, I have not had the pinching pain, and the motion seems to be getting better gradually. With that said, I still have some discomfort at times and a long way to go to recover all my motion as expected at this phase of the rehab process.
I passed a major milestone last Thursday as I hit the 6 week post-op mark. I have been transitioning out of the sling since week four (at home) while continuing to use the sling out in public. I officially quit using it last week. Things have been progressing, but two words really define the recovery so far: slow and incremental.
Being patient is no easy task when I am so used to working in the clinic, lifting weights and playing sports with my boys. Sleeping has still been a bit of a challenge as the shoulder aches after a few hours in one position, but I am now sleeping in my bed for 6-7 hours with only 2 disturbances per night. My mobility with dressing, shaving, showering and getting dressed is steadily improving. With respect to pain, it is absent at rest. However, it still strikes when I move the wrong way or happen to lift the arm against gravity due to weakness and stiffness.
Rehab
I have been going twice per week, but missed last week due to a summer vacation. I was diligent with my exercises 2x/day while away. Prior to leaving, my latest passive range of motion was equal to 117 degrees of flexion and 38 degrees of external rotation at 5 weeks post-op. As far as guidelines for the next 2-4 weeks, the goals are to restore ROM, resolve pain and begin light strengthening with rehab activities such as:
- Begin active assistive range of motion (AAROM) progressing to active range of motion (AROM)
- Continue with deltoid and rotator cuff isometric strengthening
- Begin light scapular strengthening – retraction (light rows), protraction (serratus anterior work), scapular depression and gentle ball stabilization work in a dependent position
- AAROM exercises with a dowel rod or cane (external rotation, extension, scaption, flexion, horizontal adduction/abduction)
- Joint mobilization, continued passive stretching to restore full range of motion and addition of shoulder pulley in this phase
- Light biceps and triceps strengthening (elbow at side)
- Scar massage
One important note: I have found the continued use of ice helpful in reducing daily soreness and discomfort following my home program. As such, I would highly recommend its daily use this late into the rehab.
For those following along with my post-op journey, this marks days 15 – 21. I saw the MD for my first post-op follow-up on Friday June 4 (day 15 post-op). He told me I could get rid of the pillow that came with my sling. I was thrilled as it is summertime and that thing was bulky and hot.
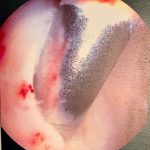
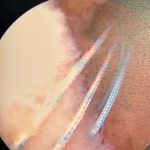
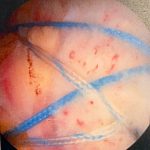
Surgical pictures
- Large bone spur
- 1 cm tear in supraspinatus
- Anchor
- Sutures
- Finished repair
You can see from the bone spur outlined in red above that my tear was an caused by repetitive micro trauma over time. Eventually, the tendon became tattered and torn. All the years of weight training probably contributed to some of this, as well as my type 2 acromion. I ended up with three total anchors and a suture bridge repair.
Rehab
I wish I could say all my years stretching patients made rehab easy for me, but that is not the case. Stiffness, weakness, soreness and atrophy were now a reality for me. My external rotation motion was beginning to improve, however, overhead flexion continued to be painful and stiff. My PT could get me to about 90 degrees of flexion while laying on my back, but with a significant amount of discomfort. It was more comfortable in the scapular plane.
The visits consisted of:
- Heat x 10 minutes
- Pendulums
- PROM by the PT for about 30 minutes – external rotation (ER) and scaption
- Passive cane ER in scapular plane and seated
- Table slides and seated forward bow (more in scapular plane)
- Active side-lying scapular movement – elevation, depression, protraction/retraction
- Scapular retractions (shoulder blade squeezes)
- Game Ready
For those following my rehab journey, this entry will recap days 8-14 after surgery. At this point, I had been off pain meds for 4 days. However, I will admit I took one pain pill prior to my first PT session exactly one week out from surgery. For two decades I have listened to patients recount stories of their own or friends who report how painful therapy is after this surgery. Oddly enough, most of my patients over the years said it was not so bad. Perhaps, there is great variability in the intensity of the passive stretching among therapists.
Research Nuggets
The literature offers support and caution for early motion after rotator cuff repair. While ROM is generally better early on with early motion, there is some concern about higher re-tear rates. I am in the camp that gentle early passive range of motion (PROM) is okay given the proper regimen and patient compliance. Early active range of motion (AROM) or too vigorous PROM is likely to be more detrimental to the repair. Ultimately, these decisions are made based on the size of the tear, tear configuration, patient’s health and age, MD preference and whether or not this is a primary or revision repair.
The article abstract below is a great reference for activities and activation of the rotator cuff as measured by surface EMG to provide some insight for patients and clinicians regarding safe movement and exercise in the rehab process:
https://pubmed.ncbi.nlm.nih.gov/28704624/
In addition, here is another article that outlines post-op rehab (you can download the entire article for free)
https://pubmed.ncbi.nlm.nih.gov/29399735/
My First PT Visit
So, I would be lying if I said I was not nervous. I mean I was always the guy stretching the fresh post-op shoulders, and suddenly I am the one laying on the table a week out from surgery about to let someone move my stiff, sore shoulder. Fear of the unknown is probably the worst in that moment. My therapist is a colleague in my own clinic who actually reports to me. No pressure on him, right? LOL
He and I agreed to co-pilot my rehab and map everything out through constant dialogue and feedback. He has done a good job thus far. That first day the shoulder felt like a cement block to me. It seemed like super glue was preventing it from moving much. The focus was on gentle external rotation and flexion range of motion. Both hurt, but the flexion was by far the worst for me.
After doing pendulums and the PROM with him, my routine consisted of:
- Seated passive external rotation using a cane on my own – 2 sets of 15
- Scapular retraction (gentle squeezing of the shoulder blades together) – 2 sets of 15
- Seated table slides with a towel – 2 sets of 15
- Game Ready x 15 minutes with low compression
Last week I began sharing my story about my left arthroscopic rotator cuff repair. As reminder, I had surgery on May 20. In this post, I will share more about the first week. I get many common questions like: How bad does it hurt? When can you get rid of the sling? How long is the total recovery?
The entire outpatient procedure went well. I barely remember getting an interscalene block (kudos to the anesthesiologist) and the entire operation lasted about 45 minutes. The oldest feeling is not feeling the left arm and having no control of the arm until the block wears off. The entire arm is essentially paralyzed and numb. Great for pain management to be sure, but not even being able to use the hand is inconvenient for small prehensile tasks.
I was fortunate that I did not have any adverse reaction to the anesthesia itself. I was a bit tired and groggy for the first 4-6 ours after surgery. The biggest adjustment is getting used to the sling and abduction pillow (see below)

Learning how to sit, adjust and take this off/put it on takes some getting used to. However, I quickly learned how valuable and supportive it was once the block wore off. My surgery was at 8:45 AM on a Thursday. The block wore off about 18 hours later at 3 AM. Let’s just say that aha moment was enough to get my attention.
Pain
I would say pain level was 7/10 for me. The doctor and his staff had advised me to start taking pain pills ahead of the block wearing off and I had initiated that about 8 hours after surgery. I was alternating ibuprofen every 2 hours while taking oxycodone every 4 hours. I can only imagine how much more it would have hurt if I had waited for the block to wear off.
Cryotherapy
The first 3-4 days afterward were the worst in terms of pain. Generally, pain at rest was probably 3-4/10, occasionally spiking to 9/10 if I moved the wrong way. Aside from the meds, I used cryotherapy, specifically a Game Ready, extensively (20 minutes on, 40 minutes off) 8-10 times per day the first week. I cannot say enough about how helpful this is in managing pain and inflammation.
- Game Ready unit
- Shoulder sleeve
This unit provides cold and compression, however, I would recommend low or no compression initially as your incisions will be tender, especially once the surgical dressing is removed at day 3 post-op. I sat upright in a chair and supported the elbow while using this machine. The hospital or outpatient facility will offer a polar care unit for $250, but I opted for this unit as I have used it for years in the clinic, while hearing countless patients tell me how much better it is. A 3-week rental will cost you $300, but it is well worth it.