Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Many athletes and clients struggle with hamstring muscle activation. A normal quad to hamstring ratio would be 3:2, but studies often find that subjects tend to be closer to 2:1 (especially females). This diminished ratio can increase knee injury risk (non-contact ACL) with jumping and cutting sports. Some people struggle with proximal hamstring tendinopathy related to overuse. Incorporating eccentric hamstring exercises in your training can markedly improve hamstring strength and activation patterns.

Quad/Ham dynamic relationship
Execution: Begin in supine with 90 degrees of knee flexion and the feet flat on the floor. Next, bridge up into a table top position. Then, slowly begin to walk the feet out keeping the weight on the heels in an alternating pattern. Move the feet as far away from the body as possible while maintaining a good static bridge position.
Once form starts to falter or fatigue sets in, walk the feet back in using the same cadence and incremental steps until the start position is achieved. Perform 5 repetitions and repeat 2-3 times. Focus on control while avoiding pelvic rotation, and be cautious working into too much knee extension to avoid poor form or cramping.
This is an excellent way to improve hamstring strength while emphasizing pelvic stability. This exercise should be preceded by static bridging to ensure the client understands how to maintain a neutral pelvic position (consider using a half roll or towel as a visual aid to cue him/her out of rotational movement initially). The walk out exercise can be implemented as part of ACL prevention/rehab programs and also works well for runners and athletes struggling with hip/pelvic stability, proximal tendinopathy and general posterior chain weakness.
Regression: Bridge up and march in place for repetitions or time to develop sufficient strength and stability.
Progression: Increase repetitions or slow the cadence down pausing longer at each step to increase time under tension. Additionally, move the hands from palm down to palm up to reduce stability. For advanced clientele, the arms could be crossed with the hands resting on the opposite shoulder.
This is the fourth corrective exercise I have featured in my “Functionally Fit” online column for Personal Fitness Professional Magazine. All of the correctives are based on screening assessments from the FMS.
The active straight leg raise (ASLR) assessment (as part of the FMS) is an essential part of any assessment I do on my athletes and runners. It provides a great look at a client’s ability to stabilize their spine/pelvis and we observe hip separation with one hip moving into flexion and the other fixed hip moving into greater relative extension.
Why does hip disassociation matter? Simply put, a lack of ideal separation can negatively impact step and/or stride length, reduce propulsion and create other compensations that increase energy expenditure and reduce overall running form. Some deviations that may occur include hip drop, increased rotation or circumduction of the swing leg, excessive torso rotation, increased knee flexion and diminished stride length to name a few.

Execution: Lie on your back. Using a doorway, place one leg against the doorway in a position that allows you to keep the lumbar spine flat while the other leg is extended and on the floor. Next, flex the down hip to the height of the other fixed leg extending the knees. This leg will remain unsupported. Now, point the toes of the unsupported leg and reach out toward the ceiling. Slowly lower the leg to the floor or the lowest point where you can still maintain a neutral lumbar spine (a bolster may be placed beneath the leg if needed). Perform 10 repetitions and repeat 2-3 sets on each side.
Progress the activity by lowering the leg further and/or sliding closer to the doorway to increase the hip flexion and total hip separation. Do not allow the lumbar spine to extend as this is a common compensatory motion for limited mobility in the iliopsoas.


Application: This activity will improve active mobility of flexed hip as well as promote continuous core stability and available hip extension of the opposite hip. It challenges the client’s ability to disassociate the lower extremities while maintaining stability in the pelvis and core. Keep in mind it is more than just a hamstring flexibility activity as it also addresses static (pelvis/spine) and dynamic (hip) stability in asymmetrical hip separation pattern.
This separation pattern is essential for optimal running mechanics. Poor hip disassociation can lead to asymmetrical or bilateral movement flaws, thereby reducing performance and leading to compensatory motion with an elevated risk for injury. This simple technique can be done daily to enhance hip mobility and pelvic/hip stability.
Perhaps one of the most researched topics is ACL injuries. I have been studying and working for years in my clinical practice to find the best ways to rehab athletes following injury as well as implement the most effective injury prevention strategies. Prior studies indicate prevention programs even when self directed can be successful.
However, on the whole injury rates have not declined over the past decade or so. Much attention has been given to valgus landing mechanics, poor muscle firing, stiff landings, genetic difference between males and females, ligament dominance, quad dominance, and so forth. The predominant thoughts today for prevention center around neuromuscular training and eliminating faulty movement patterns (refer to work being done by Timothy Hewett and Darin Padua).
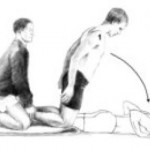
We also know from a biomechanical standpoint that the hamstrings play an integral role in preventing excess anterior tibial translation, and as such hamstring strengthening needs to be a big part of the rehab and prevention program. I believe in hamstring training that allows for activation in non-weaightbearing and weight bearing positions. Common exercises I will use include:
- HS bridging patterns (double /single leg, marching, knee extension, stability ball)
- Nordic HS curls
- HS curls (stability ball, TRX or machine)
- Sliders – focus on slow eccentric motion moving into knee extension followed by simultaneous curls/bridge
- Single leg RDL (add dumbbells or kettle bells for more load)
Note: click on any of the thumbnail images above for a full view of the exercise. From left to right: Nordic HS curls, sliding hamstring curls and single leg RDL).
A recent blog post entry by the UNC Department of Exercise and Sport Science (@UNCEXSS) has spurred my post today. Click here to read their entry on optimizing injury prevention based on work done by Professor Troy Blackburn regarding the effect of isometric and isotonic training on hamstring stiffness and ACL loading mechanisms. The research that was done holds promise for hamstring training designed to increased musculotendinous stiffness (MTS).
This post is the third corrective exercise in a series I am doing for Personal Fitness Professional Magazine in my online column titled “Functionally Fit.” To read more online exercise tips, visit www.fit-pro.com.
The hurdle step assessment (as part of the FMS) is designed to challenge the body’s proper stepping and stride mechanics as well as stability & control in single leg stance. The step leg must perform ankle DF and hip/knee flexion while core stability must be present in single leg stance.

Limited hip mobility and/or poor hip and core stability restricts natural movement and leads to compensatory motion often in the form of unwanted hip rotation, hip hiking, trunk sway in the frontal and sagittal plane. A common corrective exercise prescribed to improve core stability is a standing march (single leg stance) with straight arm pulling to engage the core.
Execution: Begin standing with the feet together while holding the cable handles with the palms down. Select a weight that provides ample enough resistance to maintain isometric shoulder extension for 30-60 seconds. Be careful not to select too little or too much weight as this will disrupt the execution of the exercise.
Next, pull the arms down toward the side and hold in that position. Maintaining an erect posture, slowly lift the left leg up (ankle dorsiflexion with knee and hip flexion) and pause for 2-3 seconds. Move the unsupported leg back to the start position but keep the arms actively extended. Repeat this sequence for 10 times on the left leg. Rest for 30-60 seconds and then repeat on the other leg. Perform 2 sets.

Additional notes: I tend to focus on unilateral consecutive repetitions (as described above) especially if there is a 2/1 asymmetry with the hurdle step. As the asymmetry is resolving, I will progress to a reciprocal pattern as this is more natural in life/sport. If a cable column is unavailable, alternate methods include using a suspension training apparatus or resistance tubing anchored high enough to accomplish the same upper body isometric pulling.
Application: Poor hip stability and control in single leg stance is a common cause of overuse injuries in runners and contributes to increased risk for anterior knee pain and ACL injuries. Keep in mind that poor performance on the hurdle step movement can be related to weak hip flexors on the stepping leg, tight hip flexors on the stance leg, diminished hip stability and poor balance.
It is critical to assess the whole movement prior to assuming that there is just one problem or weak link in the kinetic chain. Restoring symmetric, optimal stepping patterns will promote proper hip disassociation, as well as training the body to synergistically activate core and hip musculature to demonstrate optimal single leg stability in unilateral stance.
Every year I like to look back and reflect on things I have learned, things I have changed my mind about and of course clinical pearls that stand out. Over the past year, I have been sharpening my IASTM skills, begun to practice dry needling techniques, and scrutinizing my hip and core exercises that I routinely use in rehab.
I look forward to sharing more about my clinical experiences with dry needling in 2014, but I feel the most critical and recurring theme of 2013 has been the overwhelming impact I have seen poor ankle dorsiflexion have on my patients. I treat scores or runners, triathletes and clients with knee pain. The most common issues in this group of clientele tends to be IT band friction syndrome or patellofemoral pain.
When I assess this group of patients, I routinely find the following:
- Poor dorsiflexion
- TFL dominance
- Glute weakness
Any time I evaluate a runner, I assess closed chain dorsiflexion (DF) mobility. This can be assessed in half kneeling on the floor or standing at a wall. I suggest removing the shoes during the assessment to eliminate any rise from the heel in the shoe that may bias the movement. In addition, I hold the ankle in subtalar neutral to get a true assessment without allowing pronation.
The image below simply demonstrates the assessment position as well as the corrective exercise that can be used to facilitate better motion.

Clients should be able to attain about 5 inches of clearance beyond the toes without lifting the heel or relying on pronation to get there. I routinely see limited mobility, and more importantly almost 100% of the time I find asymmetry on the side of the affected knee.
I recently evaluated a 29 y/o active female client who does Crossfit 3x/week and likes to run. She has not been running much due to chronic right lateral knee pain and medial calf pain. Her goal is to get back to running half-marathons. Upon evaluation, her overhead squat assessment revealed pronation and external rotation bilaterally, right greater then left. Her standing wall DF assessment revealed nearly a 1 inch deficit on the right side (about 3 inches), while her left side was 4 inches.
Below is how she looked on the treadmill video analysis I performed:

You can see the highlighted areas in the photo above. She has a marked amount of pronation in mid stance as well as left pelvic drop due to poor gluteal activation. The poor hip stability and activation on the right side also plays directly into TFL dominance with the repetitive femoral internal rotation and adducted position of her right hip..
This poor biomechanical chain is set into motion by poor dorsiflexion mobility. Runners can get away with this for shorter distances (3-4 miles) in many cases, but increased mileage leads to shin splints, calf strains, IT friction syndrome and patellofemroal pain. You can see how this poor kinetic chain movement leads to ongoing microtrauma and eventually debilitating pain and dysfunction. No matter how much one rests, going back to higher mileage will yield the same result.
In my client’s case, she also had a trigger point in her medial soleus – another issue connected with the ankle mobility problem. Her primary treatment plan will focus on soft tissue mobilization for the gastroc/soleus complex, TFL/ITB and glutes/piriformis, ankle dorsiflexion mobility exercises, IASTM to her gastroc/soleus/Achilles, single leg balance and strengthening and hip/core activation and stability work.
I am confident all of this will effectively resolve her pain. However, it all begins with restoring ankle mobility. They say a picture is worth a thousand words. I strongly believe the picture I included of my client on the treadmill speaks volumes as to how poor ankle mobility can lead to unwanted compensatory motion, gluteal inhibition and overuse injuries. The take home message here is be sure to assess ankle mobility in the presence of any lower extremity pain or dysfunction as it is often a critical piece of the puzzle in the face or recurring injury and chronic pain.