Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Core strength and stability deficits are apparent in many people. The ability to restrain movement while keeping a stable base or pillar is essential for injury prevention. Building prerequesite pillar (hips, torso and shoulders) stability is important before loading a pattern and moving more explosively. This exercise I recently featured for PFP Magazine incorporates a progression for both options.
Application: Poor hip, trunk and shoulder stability elevates injury risk with daily activities and sport. This movement introduces controlled hip extension, torso rotation and shoulder elevation, while aiming to improve pillar strength and stability. The handle bar moves around the bar facilitating a safe and smooth motion. Using both hands allows for more control initially allowing the client to incrementally adjust the amount of rotation while they learn to move in a 3D manner. Working in a slower manner will effectively train anti-rotation strength /control as well.
The exercise progression provides an option to train explosively to develop power from the ground up using both upper extremities similar to a push press except introducing some rotation to the movement. Overall, this exercise offers a great way to train the entire kinetic chain in a multiplanar fashion.
Precautions: Clients with any existing rotator cuff and/or labral pathology or low back dysfunction should proceed with caution initially mastering controlled form with light loads and not push through any discomfort. Be sure to use proper body mechanics when lifting the bar off the ground as well.
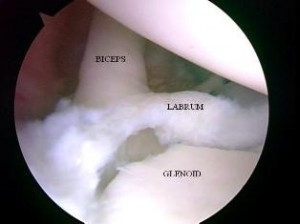
SLAP tears are a common problem for overhead athletes among others today. There is no consensus per se in how to treat them and results following primary repair are mixed. Common complaints following a repair are persistent pain and stiffness. In the past, I have writtne about SLAP tears as well as outcomes for elite pitchers.
In addition, I have discussed outcomes for type 2 SLAP tear revision surgery on this blog. What always concerns me (and more importantly patients who undergo surgery is how to achieve predictable pain relief and recover shoulder function. In the April 2014 edition of the American Journal of Sports Medicine, there is a level 4 prospective study by McCormick et al. looking at the efficacy of subpectoral biceps tenodesis as a viable solution for failed primary SLAP repairs. The study took place from 2006-2010 and all procedures were performed by 2 fellowship trained surgeons at a tertiary military facility.
Subjects: Active-duty men and women b/w 18 and 50 years old who had arthroscopically confirmed type 2 SLAP lesions and who then underwent arthroscopic repair and were subsequently unable to return to duty(follow-up period was 2-6 yeaers with mean follow-up of 3.5 years). They also had to consent to a biceps tenodesis to address the failed repair. All told, 42 of 46 patients completed the study. The mean age was 39.2, while 85% of the subjects were male.
Criteria to be included in the study: inability to return to active duty within a minimum 6 months of surgery, ASES score less than 75 at 1 year follow-up from the primary procedure, or patient electing to undergo revision surgery due to dissatisfaction with the primary results.
Procedure: Biceps tendon was released and the remaining stump was debrided so the superior labrum was confluent with the remaining labral tissue. All sutures and loose anchors were removed. If the rotator cuff interval was inflamed, debridement with a 4.o mm shaver was used and/or radiofrequency wand was used. Next, a 2 cm incision was made in the axillary skin crease at the inferior border of the pec major. The biceps tendon was anchored 1 cm proximal to the musculotendinous junction using a nonabsorbable suture and 8 x 12 interference anchor fixation.
Rehab protocol: Patients were in a sling for 4 weeks with no active biceps use for 6 weeks. They all underwent graded supervised physical therapy consisting of an initial 6-week phase of passive ROM exercise in addition to scapular and core strengthening. This was followed by progressive strengthening at 6 weeks and return to-duty-evaluation at 3 months post-op.
Results
- 34 patients (81%) returned to active duty
- Clinically significant improvement across all outcome measures after revision surgery as follows:
- Pre-op ASES = 68 and post-op ASES = 89
- Pre-op SANE = 64 and post-op SANE = 84
- Pre-op WOSI = 65 and post-op WOSI = 81
- Pre-op shoulder flexion = 135 and post-op shoulder flexion = 155
- Pre-op shoulder abduction = 125 and post-op shoulder abduction = 155
Summary
Currently, there is no standard of care for failed SLAP repairs. One previous case control study by Boileau et al. found higher satisfaction in those undergoing biceps tenodesis compared to arthroscopic repair in the management of an isolated SLAP tear. Further, in the Boileau study there were no failed tenodesis procedures and those opting for that as revision had a full return to previous sports activity. This prospective study by McCormick et al. resulted in similarly high rates of return to previous activity and clinically significant improvements in outcome scores and ROM.
There are several reasons why primary SLAP repairs may fail including: postoperative stiffness as a result inadvertent restriction of physiological biceps excursion or nonanatomic biceps anchor reduction, suture anchor pullout, suture granuloma formation, suture pullout, synovitis, glenoid osteochondrolysis from prominent hardware, a suprascapular nerve injury (due to prominent mendial hardware placement), and a delaminated long head of the biceps.
It is also important to keep in mind the anterior-superior labrum and glenoid are poorly vascularized, and this is thought to limit the healing process. Persistent pain may manifest after surgery in light of the fact the proximal intra-articular portion of the long head of biceps tendon contains sensory and sympathetic fibers associated with shoulder pain. The authors’ findings at the revision procedure in this study suggest a consistent constellation of multifactorial complicating factors including: synovitis of the rotator cuff interval, loose knots, and a lack of healing at the glenoid interface.
Key takeaways
- Outcomes following primary SLAP repairs are inconsistent and patients often continue to c/o persistent pain and stiffness
- Military personnel (an extremely active population) had excellent results with a tenodesis procedure
- The results of this study cannot be generalized to the general public nor overhead athletes per se
- This study did not employ randomization nor did it compare the tenodesis to another procedure/modality so further research should be done on this
- Biceps tenodesis seems to provide a safe and effective treatment option for failed SLAP repairs at a minimum of a 2 year follow-up in active individuals
References
Boileua et al. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929-936.
McCormick et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;(42):820-825.
The shoulder mobility screen in the FMS often reveals side-to-side asymmetries. It is more common to see hypermobility in female clientele, while their male counterparts exhibit more hypomobility. Overhead athletes tend to demonstrate excessive horizontal external rotation and a relative loss of internal rotation on the dominant side. This hypomobility can be detrimental to overhead athletes and increase risk for overuse injuries if it becomes excessive.
The following exercise is an effective way to improve shoulder mobility and optimize function. One important point is to focus on form and move very deliberately through the motion.
Execution: Begin lying on the floor face up. Bend the left knee up to 90 degrees and cross the right leg over top of the left interlocking them. Roll to the left side and pin a folded towel or pad between the right knee and the floor. Place the arms in 90 degrees of shoulder flexion with the right on top of the left in an outstretched position. Next, slowly sweep the right arm up overhead and around the body as you attempt to place the torso/back on the floor. The finish position for the right arm will be reaching the right hand and arm up behind the back.
Exhale as you perform the sweeping motion and hold the end position for 2 seconds. Reverse direction and return to the start position. Perform 5-10 repetitions on each side.
Application: Limited shoulder mobility is a common finding, especially among male clientele with tightness in the pecs, lats and posterior shoulder. Asymmetry with respect to mobility is common with greater difficulty found trying to reach the dominant arm up behind the back on the FMS shoulder mobility screen. This exercise will help improve thoracic spine motion and shoulder mobility. The focus should be on strict form and proper stabilization to avoid unwanted motion. Pinning the pad (or towel roll) to the floor will help ensure better stabilization.
If hypomibility is an issue and clients score a 1, foam rolling the pec minor/major, latissimus dorsi and the posterior rotator cuff musculature prior to performing the exercise will be helpful. Stability training can be added in later once the soft tissue mobility restrictions and movement pattern is improving.
Soft tissue tightness and restriction in the latissimus dorsi is a common problem in overhead athletes, throwers, weight lifters and Crossfit participants. I often educate clientele on self myofascial release techniques using a trigger point ball or foam roller. But, I also like using a partner technique with the Stick.
Begin in standing grasping the frame of a squat rack. You may also elect to hold both handles of a TRX. Next, slowly squat down and lean back allowing the shoulders to move into flexion. Once in position, the trainer or workout partner will use the Stick to apply pressure and roll up and down along the latissimus especially working on the soft tissue near the shoulder.

Perform this technique for 30-60 seconds and then switch sides. Adjust pressure and location based on feedback from the client.
In the past, I wrote a post about Crossfit and shoulder pain based on a 38 y/o male client of mine. Click here to read that post. In my prior entry, I discussed differential diagnosis of rotator cuff and labral pathology, as well as my treatment approach for that client.
If you follow my blog, twitter feed or webinars, you know I treat a lot of Crossfit athletes. Recently, I worked with a 25 y/o female suffering from marked shoulder pain that was keeping her out of the gym.

Below are the key findings from her intake on 8/30/13:
- Onset of left shoulder pain on 8/8 related to snatches
- Right hand dominant
- Intermittent pain if sleeping on her left side
- Full AROM
- Mild weakness with supraspinatus and external rotation on left
- Positive impingement signs
- Positive O’Brien’s test (labral test)
- Positive sulcus sign bilaterally (indicates multi-directional instability or MDI)

Sulcus sign
Treatment intervention
- Rhythmic stabilization and PNF exercises
- Rotator cuff and scapular strengthening
- Closed chain stabilization training
- Game Ready (cryotherapy)
- Home program issued at visit #1
I saw the patient once per week and she did her home program for 4 weeks. At week 4, we gradually began allowing her to do some modified gym workouts but still no snatches or full overhead work. She was pain free at this time and all impingement/labral signs had resolved. At this point she returned to some wall ball drills (limited height) but still no snatches.
The client’s final visit was on 10/2/13. Her Quick Dash percentage of perceived shoulder dysfunction was now 0%. She was symptom free, but more importantly she had a great understanding of how to modify her lifts, loads and volume based on her multi-directional instability. She was now aware of how her instability impacts her shoulder in “at risk” positions and in the face of fatigue. This brings me to the primary reason for this second post related to Crossfit and shoulder pain.
In my initial post, I focused on overuse and shoulder inflammation as a result of poor mobility, muscle imbalances and a lack of physical preparedness to do high intensity exercise like Crossfit. On the other end of the spectrum lies the unstable shoulder.
Hypermobility and/or shoulder instability is a major problem for those doing Crossfit in light of the following:
- Many lifts and exercises put the shoulder in “at risk” positions
- Poor glenohumeral joint stability places more stress on the rotator cuff and long head of the biceps
- With the AMRAP approach and train to failure nature of the WOD, fatigue is a given and this means the stabilizing muscles that matter most will often fail leading to a much higher injury risk
Key Takeaways
- My client had secondary rotator cuff and bicipital irritation related to primary instability
- Rest and a combined stabilization and cuff/scapular strengthening exercise program was effective in resolving her symptoms within 30 days
- High load/high volume overhead lifts and those that place the shoulder at end range pose a higher injury risk for those with MDI or anterior instability
- Shoulder stability work trumps mobility work in those with shoulder instability – this often runs counter to traditional approaches that tend emphasize better mobility (one program does not fit all)
Closing thoughts
We must keep in mind that the shoulder is inherently unstable in order to allow us the freedom of movement necessary to perform the various tasks and exercise. With that said, repetitive movements and lifts can create micro and/or frank shoulder instability over time. Those with a history of shoulder subluxation/dislocation/instability are a high risk group to begin with. Adding high loads to failure places the shoulder in a fatigue and compromising state. As a coach, competitor or health professional, we must remember that even the best intentions and coaching can fail us if the risk of a lift outweighs the reward.
As I have said before, anyone who decides to do Crossfit MUST get a proper assessment prior to starting to reduce injury risk. Ideally, this assessment would begin with a full FMS to help uncover any mobility or stability issues and asymmetry. Keep in mind research reveals that females will almost always score a 3 on shoulder mobility and many may be hypermobile. Conversely, they tend to score lower (1 in many cases) on the trunk stability push-up. Any pain with screening would necessitate a referral to a PT or MD for further evaluation.
Trainers cannot be asked or expected to catch multi-directional shoulder instability. However, they can and should be aware of relative risk, anatomical tendencies and red flags that may predispose clients to injury. For those wanting to be the best in the business, I would suggest developing a system for assessing clients and partnering with allied health professionals like me to incorporate best practices in their business. Perhaps most importantly, trainers and coaches must be willing to adapt, limit, or eliminate exercise that does not fit the needs and abilities of the clientele.
The random nature of the WOD makes it difficult for unassuming clients to judge how best to fit in the Crossfit model if they have a dysfunction or injury concern. My goal is always to empower people with knowledge about their body and sound advice for optimal training. For those intent upon getting back to Crossfit after injury, I work hard to normalize their function and offer tweaks and modifications to prevent re-injury. Prehab is a must for this population. But in the end, some shoulders will simply not be able to handle the rigors and intensity of Crossfit.





