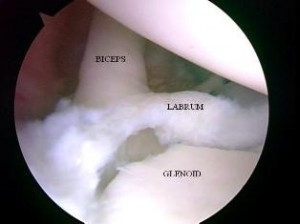
SLAP tears are a common problem for overhead athletes among others today. There is no consensus per se in how to treat them and results following primary repair are mixed. Common complaints following a repair are persistent pain and stiffness. In the past, I have writtne about SLAP tears as well as outcomes for elite pitchers.
In addition, I have discussed outcomes for type 2 SLAP tear revision surgery on this blog. What always concerns me (and more importantly patients who undergo surgery is how to achieve predictable pain relief and recover shoulder function. In the April 2014 edition of the American Journal of Sports Medicine, there is a level 4 prospective study by McCormick et al. looking at the efficacy of subpectoral biceps tenodesis as a viable solution for failed primary SLAP repairs. The study took place from 2006-2010 and all procedures were performed by 2 fellowship trained surgeons at a tertiary military facility.
Subjects: Active-duty men and women b/w 18 and 50 years old who had arthroscopically confirmed type 2 SLAP lesions and who then underwent arthroscopic repair and were subsequently unable to return to duty(follow-up period was 2-6 yeaers with mean follow-up of 3.5 years). They also had to consent to a biceps tenodesis to address the failed repair. All told, 42 of 46 patients completed the study. The mean age was 39.2, while 85% of the subjects were male.
Criteria to be included in the study: inability to return to active duty within a minimum 6 months of surgery, ASES score less than 75 at 1 year follow-up from the primary procedure, or patient electing to undergo revision surgery due to dissatisfaction with the primary results.
Procedure: Biceps tendon was released and the remaining stump was debrided so the superior labrum was confluent with the remaining labral tissue. All sutures and loose anchors were removed. If the rotator cuff interval was inflamed, debridement with a 4.o mm shaver was used and/or radiofrequency wand was used. Next, a 2 cm incision was made in the axillary skin crease at the inferior border of the pec major. The biceps tendon was anchored 1 cm proximal to the musculotendinous junction using a nonabsorbable suture and 8 x 12 interference anchor fixation.
Rehab protocol: Patients were in a sling for 4 weeks with no active biceps use for 6 weeks. They all underwent graded supervised physical therapy consisting of an initial 6-week phase of passive ROM exercise in addition to scapular and core strengthening. This was followed by progressive strengthening at 6 weeks and return to-duty-evaluation at 3 months post-op.
Results
- 34 patients (81%) returned to active duty
- Clinically significant improvement across all outcome measures after revision surgery as follows:
- Pre-op ASES = 68 and post-op ASES = 89
- Pre-op SANE = 64 and post-op SANE = 84
- Pre-op WOSI = 65 and post-op WOSI = 81
- Pre-op shoulder flexion = 135 and post-op shoulder flexion = 155
- Pre-op shoulder abduction = 125 and post-op shoulder abduction = 155
Summary
Currently, there is no standard of care for failed SLAP repairs. One previous case control study by Boileau et al. found higher satisfaction in those undergoing biceps tenodesis compared to arthroscopic repair in the management of an isolated SLAP tear. Further, in the Boileau study there were no failed tenodesis procedures and those opting for that as revision had a full return to previous sports activity. This prospective study by McCormick et al. resulted in similarly high rates of return to previous activity and clinically significant improvements in outcome scores and ROM.
There are several reasons why primary SLAP repairs may fail including: postoperative stiffness as a result inadvertent restriction of physiological biceps excursion or nonanatomic biceps anchor reduction, suture anchor pullout, suture granuloma formation, suture pullout, synovitis, glenoid osteochondrolysis from prominent hardware, a suprascapular nerve injury (due to prominent mendial hardware placement), and a delaminated long head of the biceps.
It is also important to keep in mind the anterior-superior labrum and glenoid are poorly vascularized, and this is thought to limit the healing process. Persistent pain may manifest after surgery in light of the fact the proximal intra-articular portion of the long head of biceps tendon contains sensory and sympathetic fibers associated with shoulder pain. The authors’ findings at the revision procedure in this study suggest a consistent constellation of multifactorial complicating factors including: synovitis of the rotator cuff interval, loose knots, and a lack of healing at the glenoid interface.
Key takeaways
- Outcomes following primary SLAP repairs are inconsistent and patients often continue to c/o persistent pain and stiffness
- Military personnel (an extremely active population) had excellent results with a tenodesis procedure
- The results of this study cannot be generalized to the general public nor overhead athletes per se
- This study did not employ randomization nor did it compare the tenodesis to another procedure/modality so further research should be done on this
- Biceps tenodesis seems to provide a safe and effective treatment option for failed SLAP repairs at a minimum of a 2 year follow-up in active individuals
References
Boileua et al. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929-936.
McCormick et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;(42):820-825.

