Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
It is no secret that running is synonymous with overuse injuries. Despite the best intentions, human nature craves more and more, while the competitive nature in us all to push a little harder also tends to get the best of us at times. One of the most rewarding parts of my job and profession is putting together plans that restore health and maximize performance.

The following story highlights both in an endurance athlete who I had an opportunity to work with last year. Normally I write about research, training and exercise on this blog. This post allows me to share the insight and perspective of one of my clients. I know that many of my readers have battled injuries. I am confident that this story of recovery and learning how to use the RIGHT training will resonate with you.
Click here to read about Anthony’s journey back to running
Many people struggle to activate their gluteal muscles while running, jumping or performing athletic activities. Turning on these muscles and “priming” the body to utilize the glutes in its normal neuromuscular programming is helpful in improving alignment and reducing injury potential. The band rotation exercises cue external rotation with the resistance pulling the knees toward one another.
Activating these muscles prior to doing multi-joint lifts, sprinting, plyometrics, etc. is beneficial in promoting optimal activation/stabilization in order to control excessive pronation with deceleration and eccentric training. The rotations can easily be added to the dynamic movement prep or even used as part of the normal training program. I also like to use them prior to incorporating side stepping and forward/backward walks with the bands.
The video below is one I created as part of my Functionally Fit series for PFP Magazine. It is a staple in our rehab programs and movement prep routines for our athletes at EXOS Athletes’ Performance at Raleigh Orthopaedic as well.
I am a big proponent of cryotherapy in my rehab whether dealing with acute or even more chronic inflammation. I routinely use cryotherapy with compression via Game Ready in the clinic for post-op knee surgeries, ankle sprains, rotator cuff pathology, Little League shoulder, labral repairs, etc. I was recently contacted and asked to review a cryotherapy solution on the market – Power Play. Full disclaimer: I am not affiliated with POWERPLAY in any way nor was I paid to write this review.
My intent in writing this review is to share information about the product itself and its efficacy for use in the clinic as well as for the general public. Power Play shipped me the standard kit which includes a carrying case, the cold compression ankle and knee wrap as well as the pump and wall charger. The entire package is easily portable for the ATC on the go, and works well in the clinic because it has three ports on the unit making multiple treatments for patients with various body parts a cinch.
Below is a picture of one of my patients recovering from ACL reconstruction using the knee wrap:

The different body part sleeves include gel wraps that attach to the sleeves via velcro along with a stocking to protect the skin from the wrap. POWERPLAY advises placing the wraps in the freezer or refrigerator prior to use. I noticed that if you place them in the freezer and pull them out for immediate use they are stiff and do not conform as well as desired to the body. As such, I would advise taking them out at least 10-15 minutes prior to use.
In terms of compression, the default setting on the display reading is 50 mmHg of compression. You can increase compression in 5 mm increments up to 70 mmHg. This is easily done with the touch of a single button. The compressor runs for 20 minutes and then shuts off on its own, so if you desire lass than 20 minutes you would need to set a timer (not a big deal).

POWERPLAY pump
Overall, the unit is convenient to take on the road and very easy to use. The company states it will run the unit for 8-12 hours on one charge, and I find this to be accurate so far. Patient feedback is that they like the wraps and the level of pressure, and they are comparing it to the traditional GameReady clinic cryotherapy I use with them on a routine basis. The POWERPLAY unit is also definitely cold enough and comparable to all other forms of cryotherapy we have in the clinic.
I find the entire package is reasonably priced for the overall quality and portability of the product. I think it would be a worthwhile investment for PT clinics, ATCs on the go and a client looking to have a high quality cryotherapy solution at home while recovering from an injury or surgical procedure. I have long been a fan of cold and compression so I like this product, and I look forward to trying out their shoulder wraps next! Click here to learn more about POWERPLAY.
The tensor fascia lata (TFL) is a problematic muscle for many clients. In many cases, it is synergistically dominant over the gluteus medius and often contributes to tightness associated with the IT band. Its actions are primarily hip flexion and abduction, and it tends to be tight in many runners and athletes I see. Performing targeted soft tissue mobilization can help resolve myofascial tightness as well as promote better activation and preferential recruitment of the gluteus medius.
Many people argue the effectiveness of foam rolling the IT band itself. While I am not inclined to ignore it altogether, I do believe that foam rolling probably has a far greater impact on the length/tension of the soft tissue beneath and associated with the IT band (e.g. glutes, quads, hamstrings and TFL). The TFL is often full of trigger points.
Below is a video I created for my Functionally Fit column for PFP Magazine. Employing some routine soft tissue mobilization will help reduce hip flexor tightness and help reset the neuromuscular system and set the stage for enhancing preferential gluteus medius activation during training exercises.
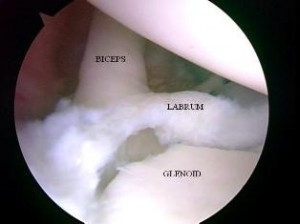
SLAP tears are a common problem for overhead athletes among others today. There is no consensus per se in how to treat them and results following primary repair are mixed. Common complaints following a repair are persistent pain and stiffness. In the past, I have writtne about SLAP tears as well as outcomes for elite pitchers.
In addition, I have discussed outcomes for type 2 SLAP tear revision surgery on this blog. What always concerns me (and more importantly patients who undergo surgery is how to achieve predictable pain relief and recover shoulder function. In the April 2014 edition of the American Journal of Sports Medicine, there is a level 4 prospective study by McCormick et al. looking at the efficacy of subpectoral biceps tenodesis as a viable solution for failed primary SLAP repairs. The study took place from 2006-2010 and all procedures were performed by 2 fellowship trained surgeons at a tertiary military facility.
Subjects: Active-duty men and women b/w 18 and 50 years old who had arthroscopically confirmed type 2 SLAP lesions and who then underwent arthroscopic repair and were subsequently unable to return to duty(follow-up period was 2-6 yeaers with mean follow-up of 3.5 years). They also had to consent to a biceps tenodesis to address the failed repair. All told, 42 of 46 patients completed the study. The mean age was 39.2, while 85% of the subjects were male.
Criteria to be included in the study: inability to return to active duty within a minimum 6 months of surgery, ASES score less than 75 at 1 year follow-up from the primary procedure, or patient electing to undergo revision surgery due to dissatisfaction with the primary results.
Procedure: Biceps tendon was released and the remaining stump was debrided so the superior labrum was confluent with the remaining labral tissue. All sutures and loose anchors were removed. If the rotator cuff interval was inflamed, debridement with a 4.o mm shaver was used and/or radiofrequency wand was used. Next, a 2 cm incision was made in the axillary skin crease at the inferior border of the pec major. The biceps tendon was anchored 1 cm proximal to the musculotendinous junction using a nonabsorbable suture and 8 x 12 interference anchor fixation.
Rehab protocol: Patients were in a sling for 4 weeks with no active biceps use for 6 weeks. They all underwent graded supervised physical therapy consisting of an initial 6-week phase of passive ROM exercise in addition to scapular and core strengthening. This was followed by progressive strengthening at 6 weeks and return to-duty-evaluation at 3 months post-op.
Results
- 34 patients (81%) returned to active duty
- Clinically significant improvement across all outcome measures after revision surgery as follows:
- Pre-op ASES = 68 and post-op ASES = 89
- Pre-op SANE = 64 and post-op SANE = 84
- Pre-op WOSI = 65 and post-op WOSI = 81
- Pre-op shoulder flexion = 135 and post-op shoulder flexion = 155
- Pre-op shoulder abduction = 125 and post-op shoulder abduction = 155
Summary
Currently, there is no standard of care for failed SLAP repairs. One previous case control study by Boileau et al. found higher satisfaction in those undergoing biceps tenodesis compared to arthroscopic repair in the management of an isolated SLAP tear. Further, in the Boileau study there were no failed tenodesis procedures and those opting for that as revision had a full return to previous sports activity. This prospective study by McCormick et al. resulted in similarly high rates of return to previous activity and clinically significant improvements in outcome scores and ROM.
There are several reasons why primary SLAP repairs may fail including: postoperative stiffness as a result inadvertent restriction of physiological biceps excursion or nonanatomic biceps anchor reduction, suture anchor pullout, suture granuloma formation, suture pullout, synovitis, glenoid osteochondrolysis from prominent hardware, a suprascapular nerve injury (due to prominent mendial hardware placement), and a delaminated long head of the biceps.
It is also important to keep in mind the anterior-superior labrum and glenoid are poorly vascularized, and this is thought to limit the healing process. Persistent pain may manifest after surgery in light of the fact the proximal intra-articular portion of the long head of biceps tendon contains sensory and sympathetic fibers associated with shoulder pain. The authors’ findings at the revision procedure in this study suggest a consistent constellation of multifactorial complicating factors including: synovitis of the rotator cuff interval, loose knots, and a lack of healing at the glenoid interface.
Key takeaways
- Outcomes following primary SLAP repairs are inconsistent and patients often continue to c/o persistent pain and stiffness
- Military personnel (an extremely active population) had excellent results with a tenodesis procedure
- The results of this study cannot be generalized to the general public nor overhead athletes per se
- This study did not employ randomization nor did it compare the tenodesis to another procedure/modality so further research should be done on this
- Biceps tenodesis seems to provide a safe and effective treatment option for failed SLAP repairs at a minimum of a 2 year follow-up in active individuals
References
Boileua et al. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929-936.
McCormick et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;(42):820-825.

