Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Let me start off by saying I have the privilege to assess and treat many avid runners on a weekly basis. Some of them are triathletes and others just dedicated runners. While the age and experience level varies, I see more female runners in all.

Recently, a woman in her mid thirties came in for PT after being referred by a physician’s assistant (PA) with a working diagnosis of hip flexor tendinitis. She had developed pain running in the past few weeks. It was now at a level preventing her from running despite using NSAIDS to reduce inflammation.
Specifically, she complained of increased pain with figure 4 sitting, difficulty and pain getting up from a chair, and increased pain with running. Her pain level at the eval was 2/10 but went as high as 9/10 with running. Lots of things can cause pain in the hip joint.

Summary of clinical findings:
- Poor single leg stance on the involved hip with mild pain
- No leg length discrepancy
- Subtle antalgic gait
- AROM for hip and L-spine are within normal limits
- No pain with quad or hip flexor stretching
- Manual muscle testing reveals 5/5 strength for hip flexion (SLR and seated), abduction and adduction
- Pain with FABER testing
- Positive hip impingement sign
- Pain with deep squat
It is no secret that proper scapula alignment and muscle activation makes for a healthy shoulder. There are many forms of dysfunction that may be present.

Generally speaking problems revolve around muscular tightness/weakness and faulty movement patterns. The term “SICK” scapula is often used and refers to Scapula Inferior Coracoid Dyskinesis. Common examples of a “sick” scapula include:
- Type I – Inferior border prominence. This is typically related to tightness in the pec minor and weakness in the lower trapezius. Keep in mind the upper trapezius will naturally dominate the lower trap in the force couple with the serratus anterior for upward rotation. You may also see increased thoracic kyphosis which will inhibit the normal resting position of the scapula.
- Type II – Medial border prominence. In this case the scapula is internally rotated or protracted and there is liekly weakness present in the rhomboids and middle trapezius. The serratus anterior may also likely be weak with evidence of scapular winging. This position places the humerus in relative internal rotation and increases risk of impingement with arm elevation.
- Type III – Superior border presence. Here the scapula appears elevated in the face of an overactive upper trap and/or levator scapulae. With active arm elevation, you may notice excessive shrugging or superior humeral head migration in light of the imbalance. Again, the lower trapezius is probably weak and being overpowered.
Click here for a great graphic display from the Journal of the American Academy of Orthopaedic Surgeons of how the scapular muscles work collectively as a force couple to promote optimal movement in the shoulder.
In many of the throwers and overhead athletes I see in the clinic, they often exhibit either medial border prominence of inferior border prominence. Additionally, I frequently observe GIRD (glenohumeral internal rotation deficit) values of 20 degrees or higher in those patients who come in with symptomatic shoulders (rotator cuff and/or labral issues). What does this mean?
Well, in a nutshell, it means addressing posterior capsule tightness in the throwing shoulder is important for avoiding internal impingement and SLAP tears. Tightness (or too much GIRD) can increase the load/tension in the late cocking phase of throwing thereby contributing to friction between the cuff and labrum, as well as excessive torsion on the proximal biceps tendon. Any excessive humeral head migration with repetitive throwing is a recipe for injury over time.
I have been a bit behind on blogging as of late. I try to aim for one per week, but I also strive to deliver sound and relevant content. Additionally, I do not seek outside contributors so finding time to write can be tricky with work and family life too. So, forgive me for any apparent inconsistency in posting. Just know that I will always try to provide valuable content. Today’s post centers around an article in the July 2012 edition of AJSM.

My work at the Athletic Performance Center has provided me an increased opportunity to work with FAI and athletic hip injuries. This is an area of evolution and growth in our field, so I find it particularly interesting to see rationale and thought processes centering around the timing, contribution and selection of hip exercises for active patients/athletes.
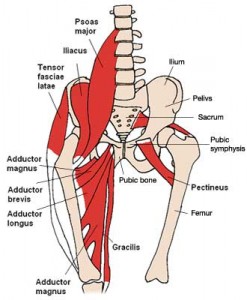
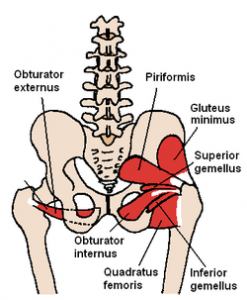
This article comes from the Steadman Philippon Research Institute in Vail, CO. The purpose of the study was to measure the highest activation of the piriformis and pectineus muscle during various exercises. The hypothesis was that highest pectineus activation would occur with hip flexion and moderate activity with internal rotation, whereas the highest activation with the piriformis would be with external rotation and/or abduction.
Methods: 10 healthy volunteers completed the following 13 exercises:
- Standing stool hip rotation
- Supine double leg bridge
- Supine single leg bridge
- Supine hip flexion
- Side-lying hip ABD with external rotation
- Side-lying hip ABD with internal rotation
- Side-lying hip ABD against a wall
- Hip clam exercise with hips in 45 degrees of flexion
- Hip clam exercise with hips in neutral
- Prone heel squeeze
- Prone resisted terminal knee extension
- Prone resisted knee flexion
- Prone resisted hip extension
All of these exercises have been reported to be used in hip rehab following arthroscopy or recovery from injury. The exercises were executed slowly and methodically with a metronome to reduce EMG amplitude variations.
Over the past several years, the trend in the health and fitness industry has been toward injury prevention and movement screening. Gray Cook and Lee Burton have given us the FMS. More recently, the Y-Balance test has emerged as another tool to assess asymmetry in the upper and lower quarter.
I am currently FMS certified and planning to attend the SFMA course next month in Durham. I routinely incorporate the FMS in both our rehab and sports performance work at the APC. I like many things about the screening exam. It provides a consistent tool to assess baseline movement and record asymmetry on a simple 4 point scale scale. It also has been shown to have good intra and inter-rater reliability. Click here for a recent study published in the Journal or Orthopaedic & Sports Physical Therapy.
For those unfamiliar with the screen, it is 7 tests scored on a 0-3 scale as follows:
- 0 = pain
- 1 = unable to perform the movement pattern (or perform with marked dysfunction)
- 2 = performs the movement with a mild compensation
- 3 = performs the movement correctly
I would say on average, most of the athletes I screen score between a 12 and 15. My highest score was a 19 (9 year old gymnast) and my lowest was a 9 (NFL lineman). As screeners, we are charged with uncovering asymmetry and faulty movement patterns. What do you see in the following picture?

Clearly, the dowel is not level, thus we score it a 2. She also had some ER in the right leg when stepping over the hurdle. She was a symmetrical 2 on the hurdle step test. This is a Division I soccer player who scored 17 on the exam.
Most of the movements seem straightforward. However, many question what the rotary stability test measures with respect to the ideal 3 score (ipsilateral movement)? It assesses an unnatural movement pattern to be sure. This athlete failed miserably on the ipsilateral pattern but scored a solid 2 with the contralateral pattern.

I have yet to test someone who can score a legitimate 3. I have seen some get a 3 on one side and 2 on the other (asymmetrical and a red flag in FMS land). As one who naturally questions things, I find myself questioning how many are truly capable of scoring a 3.
Research along with years of observation has taught me that the brain is inherently looking for the most efficient way (aka least effort) to execute movement in life. In addition, it HATES pain just like you and I so it does everything possible to avoid it including ordering the body to perform dysfunctional movement patterns.
After a painful episode, the brain often needs reminded that the body can go back to the proper movement patterns once the pain is gone. However, it often holds that painful memory and may by default lean toward a faulty movement pattern. This protective mode then ends up perpetuating a faulty movement pattern that is no longer necessary nor efficient. Over time, dysfunctional movement patterns can create further stress or harm to other segments in the kinetic chain.
So, I am always seeking ways to stimulate the body to work properly and exercises that facilitate proper neuromuscular patterning are instrumental in my rehab and training. I wanted to share two exercises that I like to utilize in my rehab and training for the shoulder. In particular, I like to employ closed chain activity to stimulate the serratus anterior as well as the other scapular stabilizers.
Below are two exercises I wrote about in my “Functionally Fit” column for PFP magazine. The first exercise shows quadruped rocking. Shirley Sahrmann mentions this in her work, Diagnosis and Treatment of Movement Impairment Syndromes. I began using it after reading her book, and I agree that it works very well for scapular dysfunction. Below is the start and finish position for the quadruped version as well as my own advanced tripod version of the exercise.
- Quadruped start
- Quadruped finish
- Tripod finish
For a complete explanation of the exercise and its application, click here to read the column.
As a follow-up to this exercise, I included an unstable progression I like to employ using the BOSU trainer. I call this the unstable tripod scapular clock. It can be done on the knees or up on the toes. I have included a quick video on this below. Again, I like this exercise for scapular work as well as core stability training.
Click here to read my PFP column on this exercise for the full description, application and regressions. The real beauty of this last exercise is the “big bang for your buck” attributes since it hits shoulder, core and hip stability all at once for those able to work at that level. I hope it works as well for you as it has for me!




