Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
I wanted to make everyone aware of two courses that I am presenting in the next 2 weeks in conjunction with Allied Health Education:

The first is a (2) hour webinar on Current Concepts in the Recognition and Treatment of Femoroacetabular Impingement tonight, August 23 from 8-10 PM. The course is intended for PT’s, PTA’s and ATC’s looking for an in-depth presentation on the condition and its management. Click here for more information.
In addition, I am scheduled to present two (1) day seminars on “Fit Knees” in Greensboro, NC on Sept. 7 and Richmond, VA on Sept. 8. This lecture/workshop event will feature my evidence based approach to injury prevention and rehabilitation for knee osteoarthritis, running injuries and ACL injuries.
The material presented in this seminar is intended to help identify knee dysfunction and implement safe and effective rehab, corrective exercise and training strategies tailored to meet the needs of each client. Attendees will learn how the presenter utilizes the FMS, Y-Balance test and other screening tools to determine limb asymmetry and imbalances. Additionally, participants will learn how to use assessment and current research to create effective training programs, facilitate the rehab process and guide post-rehab decision making. Click here for more information.
If you have further questions, feel free to post them on the blog.
Let me start off by saying I have the privilege to assess and treat many avid runners on a weekly basis. Some of them are triathletes and others just dedicated runners. While the age and experience level varies, I see more female runners in all.

Recently, a woman in her mid thirties came in for PT after being referred by a physician’s assistant (PA) with a working diagnosis of hip flexor tendinitis. She had developed pain running in the past few weeks. It was now at a level preventing her from running despite using NSAIDS to reduce inflammation.
Specifically, she complained of increased pain with figure 4 sitting, difficulty and pain getting up from a chair, and increased pain with running. Her pain level at the eval was 2/10 but went as high as 9/10 with running. Lots of things can cause pain in the hip joint.

Summary of clinical findings:
- Poor single leg stance on the involved hip with mild pain
- No leg length discrepancy
- Subtle antalgic gait
- AROM for hip and L-spine are within normal limits
- No pain with quad or hip flexor stretching
- Manual muscle testing reveals 5/5 strength for hip flexion (SLR and seated), abduction and adduction
- Pain with FABER testing
- Positive hip impingement sign
- Pain with deep squat
I have been a bit behind on blogging as of late. I try to aim for one per week, but I also strive to deliver sound and relevant content. Additionally, I do not seek outside contributors so finding time to write can be tricky with work and family life too. So, forgive me for any apparent inconsistency in posting. Just know that I will always try to provide valuable content. Today’s post centers around an article in the July 2012 edition of AJSM.

My work at the Athletic Performance Center has provided me an increased opportunity to work with FAI and athletic hip injuries. This is an area of evolution and growth in our field, so I find it particularly interesting to see rationale and thought processes centering around the timing, contribution and selection of hip exercises for active patients/athletes.
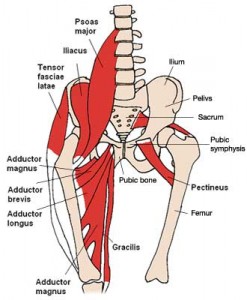
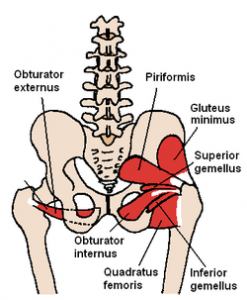
This article comes from the Steadman Philippon Research Institute in Vail, CO. The purpose of the study was to measure the highest activation of the piriformis and pectineus muscle during various exercises. The hypothesis was that highest pectineus activation would occur with hip flexion and moderate activity with internal rotation, whereas the highest activation with the piriformis would be with external rotation and/or abduction.
Methods: 10 healthy volunteers completed the following 13 exercises:
- Standing stool hip rotation
- Supine double leg bridge
- Supine single leg bridge
- Supine hip flexion
- Side-lying hip ABD with external rotation
- Side-lying hip ABD with internal rotation
- Side-lying hip ABD against a wall
- Hip clam exercise with hips in 45 degrees of flexion
- Hip clam exercise with hips in neutral
- Prone heel squeeze
- Prone resisted terminal knee extension
- Prone resisted knee flexion
- Prone resisted hip extension
All of these exercises have been reported to be used in hip rehab following arthroscopy or recovery from injury. The exercises were executed slowly and methodically with a metronome to reduce EMG amplitude variations.
Femoroacetabular impingement (FAI) is often a hidden and misunderstood cause of hip pain. I currently work with a physician who has studied under some of the best hip arthroscopists in the US, and he is performing arthroscopic procedures to resolve hip impingement. For many years, this has likely been a source of misdiagnosed, under treated and debilitating hip pain for people.
As things advance in medicine, hip arthroscopy is expanding and allowing for easier surgical correction of these issues. However, it is not an easy surgery technically speaking. As such, finding the right surgeon (if needed) is critical to attaining a positive outcome. Who normally gets it? Unfortunately, many people are predisposed to it, much like we see the natural genetic architecture (shape) of the acromion affecting impingement in the shoulder.
If you have an overhang of the hip acetabulum (socket) or non-spherical shape of the femoral head (or both) this can compromise the joint space and injure the joint cartilage and/or labrum. Destruction can occur at a very young age. I am currently rehabbing a 19 y/o male who recently underwent hip arthroscopy to debride his labrum and smooth out the hip socket and re-shape the femoral head. He had extensive damage at an early age due to his joint architecture and shows some signs of impingement on the other side as well.
How do you know if you have hip impingement? Generally, you may have hip joint pain along the front, side or back of the hip along with stiffness or a marked loss of motion (namely internal rotation). It is common in high level athletes and active individuals. However, other things may cause hip pain as well such as iliopsoas tendonitis, low back pain, SI joint pain, groin strain, hip dysplasia, etc. so a careful history, exam and plain films are necessary to confirm the diagnosis. If suspected, an MR athrogram is usually ordered to confirm if there are labral tears present. Physicians also use an injection with anesthetic to see if the pain is truly coming from the hip joint. This may be done under fluoroscopy to ensure it is in the joint space.
Signs and symptoms of FAI may include:
- Pain with sitting
- Pain or limited squatting
- Stiffness and decreased internal rotation
- Pain with impingement testing (see picture below of hip flexion, adduction and internal rotation – examiner will move the hip into this position and marked stiffness/loss of internal rotation and pain indicates a positive test)

Conservative treatment typically involves limiting or avoiding squats, strengthening the core and hip stabilizers as well as attempting to maximize mobility of the joint. Due to the fact that by the time pain brings patients in to see the doctor there has already been marked labral and joint damage, a cautious and proactive approach to managing hip pain is warranted especially in younger active patients and athletes.
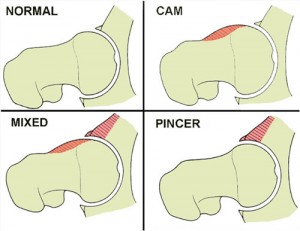
The types of lesions seen are either Cam or Pincer lesions.
Cam lesion – involves an aspherical shape of the femoral that causes abnormal contact between the ball and socket leading to impingement
Pincer lesion – involves excessive overgrowth of the acetabulum resulting in too much coverage of the femoral head and causing impingement where the labrum gets pinched
You can also see a mixed lesion where Cam and Pincer lesions are involved. FAI may lead or contribute to cartilage damage, labral tears, hyperlaxity, sports hernias, low back pain and early arthritis.
The good news is that these patients typically do well post-operatively. Dr. Philipon et al reported in 2007 in the Knee Surg Sports Traumatol Arthrosc. (click here to read the abstract) on 45 professional athletes who underwent arthroscopic management of FAI with an average follow-up of 1.6 years. In this time period 78% of them were able to return to their sport.
Following surgery, weight bearing may be restricted for the first 4 weeks or so to protect the labrum if it is repaired. With a simple debridement and re-contouring of the acetabulum, weight bearing may be initiated earlier. Avoiding twisting motions and excessive external rotation is a must in the first month or so as well. Typically, impact and twisting restrictions are lifted around 3 months post-op.
In the end, proper diagnosis and treatment is necessary to preserve the hip joint and maximize function and return to sport. If you or someone you know suffers from chronic and persistent hip pain that has failed conservative treatment, then consider getting a second look to rule out FAI.

