Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
Shoulder impingement and scapular dysfunction are common issues that plague many clients. Research indicates that certain muscles tend to dominate others while other muscles fatigue easily leading to faulty movement patterns and increasing the risk for impingement. Muscle length and posture are also key factors to consider.
I like to use a mini-band retraction with clients exhibiting excessive scapular abduction. In the video below, you will see a simple, yet effective exercise to address this faulty alignment of the scapula. Keep in mind, you must observe the client or patient from behind with the scapula exposed to properly assess alignment and movement.
This exercise is designed to strengthen the middle trapezius and rhomboids. In addition, it will improve scapular stability. Scapular abduction is usually more evident with elevation from 90-180 degrees as the ratio of scapular movement to glenohumeral movement is 1:1 instead of the normal 1:2 ratio throughout since the scapula is already in an excessively abducted posture at rest.
To read more on the application and exact execution of this exercise, click here to read my column for PFP Magazine.
I work with many runners in our clinic. I often see restrictions in the soleus. While the running community is warming up to soft tissue mobilization, many runners are still resistant to embrace it routinely and engage in it more so only when they are hurt or lacking flexibility.
STM (soft tissue mobilization) should be part of every runner’s maintenance program. Why? Simply put, repetitive stress takes its toll on the body. Rolling or releasing the tissue increases blood flow, eliminates trigger points, and facilitates optimal soft tissue mobility and range of motion.
In the diagram below, you can see common trigger points in the soleus. The X represents the trigger point & the red shaded area is the referred pain caused by the trigger point.

In the case of the soleus, restricted dorsiflexion could lead to other biomechanical compensations with running. Initially, this often creates a dysfunctional and non-painful (DN) pattern. Over time, this may eventually become a dysfunctional and painful (DP) pattern forcing runners to seek medical care. The terms DN and DP come from Gray Cook’s Selective Functional Movement Assessment (SFMA).
The gait cycle is certainly altered from dysfunction in this muscle. If ankle joint dorsiflexion is compromised (a common effect of soleus restrictions), there can be increased strain on the quads and altered movement in the hip. Overpronation and excessive hip adduction and internal rotation are common compensations seen with running. Other signs and pathology that may be associated with a soleus trigger point may include:
- Plantar fasciitis
- Heel pain
- Shin pain
- Knee or hip pain
- Back pain
As such, restoring mobility is important. A recent study revealed that immediate improvement in ankle motion can be attained with just a single treatment (click here for the abstract).
So how do you effectively resolve soft tissue issues in this area? I suggest using a foam roller or better yet the footballer and baller block in the Ultimate 6 Kit for Runners by Trigger Point (see pic below)

Rotator cuff tears are common injuries, especially among active middle age men. As researchers and scientists seek for better ways to promote healing and more optimal surgical outcomes, PRP continues to get lots of attention. If you want a basic primer on PRP, click here to read one of my earlier posts on it.
In a recent study in the October 2011 American Journal of Sports Medicine, researchers looked at the effects of PRP on patients undergoing surgery for full thickness rotator cuff tears. This is the first prospective cohort-control study to investigate the effect of PRP gel augmentation during arthroscopic rotator cuff repair. Forty two patients were included in the study (average age of 60), with 19 undergoing arthroscopic repair with PRP and 23 without.
Outcomes were assessed preoperatively and at 3, 6, 12, and finally at a minimum of 16 months after surgery (at an average of 19.7 +/- 1.9 months) with respect to pain, range of motion, strength, and overall satisfaction, and with respect to functional scores as determined using multiple assessment tools. At a minimum of 9 months after surgery, repaired tendon structural integrities were assessed by magnetic resonance imaging.
Below are images defining a full thickness rotator cuff tear:

Partial (left) vs. Full (right)
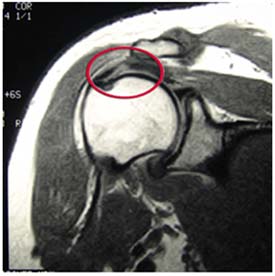
Full Thickness Tear on MRI
In my practice, I take care of many athletes ranging in age from 10 and up. Many of the injuries I see are related to over training and overuse. Common things I see in the clinic on a daily basis include but are not limited to:
- Tendonitis
- Shin splints
- IT Band Syndrome
- Patellofemoral pain
- AC joint pain/arthritis
The list can go on and on. There are many factors (inherent and training related) that contribute to such problems. I personally believe many problems can be prevented with better education, smarter training, coaching predicated on individuality and physical response, and of course adding in more recovery. Cross training is also a must – just look at what sport specialization at an early age has done to current injury rates.
You need not look any further than the declining age of patients walking through the door with what I term “repetitive microtrauma” injuries. I saw a 14 year old cross country female runner a few weeks ago who had her second stress reaction injury inside of 12 months. In addition, the rise in the number of Tommy John surgeries performed in the past decade with respect to those having them at an earlier age may serve as a harsh warning sign about doing too much too soon or doing too much of the same thing year round.
I say all this simply to say we must not be oblivious to the rise in these types of mechanical injuries. Throwing, swimming, and running are all activities that become dangerous if done in excess, and they also produce predictable injury patterns. So, if you are curious about some risk factors and how to better balance your training and manage these types of injuries, then check out a webinar I just did for Raleigh Orthopaedic Clinic last week (click on the screen shot below to view the webinar)
This presentation is ideal for athletes, parents, weekend warriors and sports coaches looking for practical, straightforward information on this topic with some foundational guidelines that can be applied objectively and immediately to injury management and recovery. If this information helps just one person avoid an injury or accelerate their recovery then I will be thrilled! Please feel free to forward this post to friends, share it on FB or tweet it!
One of the greatest things about medicine is that it continues to evolve and change. Sports medicine is at the forefront and athletes are always looking for faster ways to recover and get back in the game. If you are not familiar with platelet rich plasma (PRP) therapy, click here to read my earlier post on it.
It has been used increasingly to treat muscle strains and chronic tendinitis in the heel, knee and elbow. While some early responses have been favorable, there has not been much follow-up data or research available to assess its efficacy. In the August edition of the American Journal of Sports Medicine reports on one-year follow-up for the use of PRP in chronic Achilles tendinopathy.
The study was a double blind randomized placebo-controlled study using 54 patients (age 18-70) who had chronic tendinopathy 2-7 cm proximal to the Achilles tendon insertion (minimum of 2 months). They were randomized and given PRP or a saline injection in addition to an eccentric training program. Keep in mind recent research has indicated the efficacy of eccentric training to treat chronic tendon problems.
In this intervention, patients were given the injection with ultrasonagraphic guidance. After the injection, theyw ere told to avoid sports for 4 weeks. In week 2, they preformed a stretching program. Then all participants began a 12 week eccentric exercise program. Follow-up was done at 6, 12 and 24 weeks by one researcher, while another blinded researcher did the one-year follow-up. Clinical and ultrasonagraphic follow-up was done at each interval.
Results
At the 1 year follow-up, there was no clinical or sonagraphic benefit of PRP. This matches the findings at 6 months as well. One other radnomized studly looking at tennis elbow did find a statistical significance when they compared PRP to a corticosteroid injection at 1 year, instead of a placebo injection. Another key factor or difference is one area is load bearing and the other is not.
In reviewing this study, it should be noted that not only was pain reduction not statistically greater, nor was there any added positive tendon structure changes noted using the PRP. With that said, the looming issue with this treatment intervention is that variables like platelet count, injected volume. number of injections, preactivation and the presence of leukocytes are not always the same across studies, and they were not determined within this study either.
The takeaway here is that there appears to be no added benefit from PRP with chronic Achilles tendinits. However, there is no known negative side effect associated with trying it either. I think the hardest part is scaling back activity and being patient enough to overcome these injuries. In my experience, they often require soft tissue massage, rolling, stretching, eccentric loading, relative rest, and a very specific return-to-activity plan based 100% on the tissue and pain response of the patient.
Time and future research will continue to tell us more about PRP. I think we may find that different growth factors and treatment options may evolve that do in fact speed regeneration and healing.


