Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
One of the more challenging issues I see in the clinic is pain in the upper hamstring region. Proximal hamstring tendinopathy, referred to medically as tendinosis, is common in runners and athletes. With that said, arriving at this diagnosis can also be challenging as proximal hamstring pain can also be caused by sciatica or referred pain from the low back region. A thorough clinical exam and good history will be able to definitively help diagnose the cause.
Chronic hamstring pain can occur as a result of a previous acute tear, or due to ongoing tendinitis that is aggravated by repetitive activity. Running, biking, rowing and even prolonged sitting can aggravate the hamstring tendons where they attach to the ischial tuberosity. There is also an ischial bursa that cushions this region that can become chronically inflamed. It is a common problem for distance runners and athletes involved in sprinting, hurdles, or cutting . Typical signs and symptoms include a deep, local pain in the buttocks/upper hamstring region that worsens with running, squatting, lunging and sitting.
Differential diagnoses include:
- Sciatic nerve irritation (may be a co-morbidity in some cases)
- Ischiofemoral impingement
- Apophysitis or avulsion in adolescents
- Deep gluteal muscle tear
- Stress fracture (posterior pubic bone or ischial ramus)
- Partial or complete rupture
Proximal hamstring tendinopathy is rarely painful during activities that do not involve elastic energy transfer or compression, such as walking on even ground, standing or lying down. Tears are typically accompanied by extreme hip flexion and knee extension during an acute injury (usually hear an audible pop). In some cases, chronic pain may also be accompanied by an exaggerated pain response, referred to as central sensitization where the central nervous system conveys an amplified neural signal resulting in pain hypersensitivity.
Many people suffer from chronic hamstring pain. The question is what is the root source the pain? As a seasoned clinician, I see many patients who present with pain in the upper hamstring/ischial region. Referral sources can include the low back, hip, SI joint, proximal hamstrings, gluteals, piriformis, and ischial bursitis to name a few. In some cases, the pain can be multi-factorial as I see some runners with low level discogenic (nerve) pain and proximal hamstring tendinopathy. The sciatic nerve and its proximity with the hamstrings necessitates thoroughly vetting the symptoms and its pattern in each client. Assessing SLR, slump test, reflexes, myotomes and dermatomes is a must.
Determining what the exact source of can be difficult and requires a good subjective exam and objective testing. For the purposes of this particular post, I am focusing on the proximal hamstrings themselves as the primary source of the pain, as I see so many who struggle with proximal tendinopathy who have seen many providers with little relief.
I treat many runners and middle aged adults who experience this high hamstring or buttock pain that is often worse with:
- Sitting
- Forward bending
- Walking or running uphill
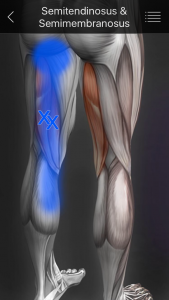
As with traditional hamstring strains, eccentric strengthening is a must for this population. However, we must consider the myofascial component and contributions to this pain as well. In many cases, these patients have ischial tuberosity tenderness. Consider the referral pattern of the medial HS illustrated below:
I typically like to consider using hip and core strengthening, dry needling, IASTM, stretching and eccentric strengthening to address the pain. If I feel the problem may include a sciatic nerve component and there is an extension bias, I will utilize some PA glides and extension exercises too. In addressing this pain pattern, we must be thorough.
A 2014 case study published in JOSPT looked at a case study with two runners (71 and 69 y/o men) who were treated with eccentric exercises, trigger point dry needling and lumbopelvic stability exercises. The rehab was phase based and the results are as follows:
Patient 1 was treated in physical therapy for 9 visits over 8 weeks. At discharge, he had achieved his goal of running 8 to 10 km 5 times each week pain free. An e-mail received 6 months following discharge noted that he had remained symptom free with all activity and that he completed a triathlon symptom free.
Patient 2 was seen in physical therapy for 8 visits over the course of 10 weeks and discharge were performed by the same therapist who performed the initial evaluations and oversaw each treatment. He was discharged after running 30 km without symptoms and reporting significant decrease in hamstring pain. The patient was seen 6 months later in physical therapy for unrelated right shoulder subacromial impingement but reported no hamstring symptoms and that he had participated pain free in a marathon.
In my practice, I have found dry needling, heat and soft tissue work to be very helpful along with stretching and strengthening. I like to use eccentric PREs and hip stability work to resolve proximal hamstring pain. Specifically, I have used the following two exercises with very good results:
Single leg RDL
Supine reverse hamstring curls using gliding discs
Both of these exercises are effective in promoting eccentric hamstring strength, hip stability, and improved hamstring mobility. Furthermore, they can be effectively used in rehab, rehab and training situations. I routinely use them in all of the above. For a more detailed explanation of the reverse curls, be sure to check out my upcoming Functionally Fit column at www.fit-pro.com.
Keep in mind that hamstring pain can be caused by one or multiple sources. It is best to seek a medical evaluation to determine the exact source of pain and address it safely and effectively. Exercises such as the ones demonstrated in this post represent a few options for addressing hamstring strains/tendinopathy. Others may include Nordic hamstring curls, prone eccentric hamstring curls and hamstring walkouts. Using manual interventions along with exercise is often effective in accelerating and optimizing full recovery.
Reference
Jayaseelan DJ, Moats N, Ricardo C. Rehabilitation of Proximal Hamstring Tendinopathy Utilizing Eccentric Training, Lumbopelvic Stabilization, and Trigger Point Dry Needling: 2 Case Reports. J Orhtop Sports Phys Ther 2014 (44)3:198-205.
I must admit that I am always looking for new ways or tools to enhance my practice and work as a sports physical therapist. I recently completed the necessary hours of training to perform dry needling in the state of North Carolina. I trained with Myopain Seminars and have nothing but great things to say about their courses.
For those unfamiliar with trigger point dry needling (TDN), it is a treatment gaining traction in the therapy world. Dry needling is a treatment that involves a very thin needle being pushed through the skin to stimulate a trigger point. Dry needling may release the tight muscle bands associated with trigger points and lead to decreased pain and improved function for those suffering from pain related to muscular dysfunction.
Trigger points may ultimately refer pain to other sites, and research indicates that TDN can reduce acidity in the muscle and clear out pain propagating chemicals. The picture below is an example of me performing trigger point dry needling to the upper trapezius of a 16 y/o female.

This particular client had been suffering from an inability to lift the arm above shoulder height and marked shoulder pain since September 2013. She also mentioned having headaches at school. Clinically, she was diagnosed with multi-directional instability and scapular dyskinesis by the referring MD. We began working on a scapular stabilizer and rotator cuff strengthening program in late November that was helping to diminish pain and increase function. However, she continued to c/o pain in school, stiffness and headaches.