Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
I rehab far too many athletes under the age of 18 with ACL tears. In many cases, I am rehabbing some who have suffered multiple ACL ruptures before they graduate from high school. The burning question is why do so many clients suffer a graft failure or contralateral injury so so often?
Is it related to genetics? Is sports specialization to blame? Perhaps fatigue and limited recovery is a problem. I think the answer is multifactorial, but to be perfectly honest we as a profession have yet to truly arrive at a consensus as to when the “right time” to return to play is. Opinions vary widely based on the athlete, sport, native movement patterns, graft choice, additional injuries (ligament, cartilage or soft tissue) and the provider.
As a clinician dedicated to both prevention and the best rehab, I am always re-evlauating my own algorithm and rehab techniques, while looking for scientific rationale to direct my exercise selection and decision making processes. A recent paper by Webster and Feller in the November 2016 edition of AJSM looked at subsequent ACL injuries in subjects who underwent their primary ACLR under the age of 20 utilizing a hamstring autograft reconstruction procedure.
So, a very common issue I see in runners is iliotibial band (ITB) syndrome. In a nutshell, it involves excessive rubbing or friction of the ITB along the greater trochanter or lateral femoral epicondyle. It is more common along the lower leg just above the knee and typically worsens with increasing mileage or stairs.
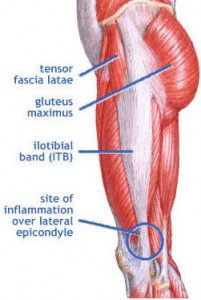
The ITB is essential for stabilizing the knee during running. Several factors may contribute to increased risk for this problem:
- Muscle imbalances (weak gluteus medius and deep hip external rotators)
- Uneven leg length
- High and low arches
- Increased pronation leading to excessive tibial rotation = friction of the band
- Improper training progression
- Faulty footwear
- Poor running mechanics
- Limited ankle mobility (specifically dorsiflexion)
- Tightness in the tensor fascia latae (TFL) and glute max
Related information on this topic include a 2010 study published in JOSPT on competitive female runners with ITB syndrome:
Click here to see the abstract of the study
Click here to read an earlier blog post analysis of the above research article
Common signs and symptoms include stinging or nagging lateral knee pain that worsens with continued running. Hills and stairs may further aggravate symptoms. Some runners even note a “locking up” sensation that forces them to stop running altogether. How do I treat this?
If you read my blog, then you know I contribute a column for PFP Magazine. I have been doing a series for them on TRX training as of late. My most recent column included an incredibly challenging exercise incorporating a plank and push-up.
Time is precious for many of us in the gym, so I am always looking for the best return on my time with each and every exercise I choose. While this one is not for the novice or inexperienced TRX user, I assure you it will be one you will love to hate! Scroll down to check out the column and see how many you can crank out before you fatigue.



Click here to read how to correctly perform the exercise, use a progressive build up series and understand the functional application. I hope you enjoy this as much as I do!
Finally, I want to wish all my American readers a Happy 4th of July!
One of my favorite tools I use in the gym with my clients is the BOSU. Admittedly, it is really easy to get carried away with various tools and equipment when training clients or ourselves. But, the BOSU is awesome if you are into building strong stable shoulders and safeguarding them against injury.
Many people focus on open chain (the hand is free in space) shoulder training, but in overhead athletes such as swimmers, volleyball players and throwers, it is essential to build a solid level of scapular strength to absorb force and enable the shoulder to move freely and effectively generate power.
I routinely include BOSU stability work in the following ways:
- Dynamic warm-up
- Core training
- Upper body work & scapular strengthening
One of my favorite exercises is what I term the “BOSU clock.” I wrote a column on this exact exercise for PFP Magazine a few months back.

Click here to read more and learn how to use this exercise to improve shoulder stability and reduce pain and/or injury risk related to shoulder instability, rotator cuff pathology and muscular imbalances.
This is just one great way to use the BOSU in your training. If you are interested in getting your very own BOSU, head on over to my OpenSky Shop and check it out – http://brianschiff.theopenskyproject.com/
In the last post, I identified the issue I believed to be going on with player x. Keep in mind the player returned to see me the week of 12/15 intially. The first line of treatment for PF issues in most clinical scenarios involves the following:
- Rest
- Ice
- Stretching (quads, hamstrings, IT band and hip musculature)
- Straight leg raises
- Short arc quads (mini-knee extensions from 30-0 degrees if you will on a bolster) although I am not a huge fan of these
- Mini-squats
- Calf raises
I advocated relative rest, ice and stretching with my athlete in addition to the following exercises initially:
- Single leg step-downs (side progressing to front version) in pain free range
- Single leg stiff legged dead lifts
- Single leg bent knee floor hamstring bridges
- Lateral ankle band walks for gluteus medius work
- Multi-planar lunges in pain free range of motion
She did well with all of the exercises after week one but noted pain with front step-downs and deeper lunges. On 12/22 I made a significant discovery: she had adopted a compensatory hip strategy to avoid normal knee kinematics with deceleration. What am I referring to? I call it a quad avoidance lunge pattern. She would shift her trunk into extension with foot contact when lunging onto the affected knee as a result of anticipation of pain. (See video clip below as I show a normal lunge pattern, a quad avoidance lunge pattern and the exericse I use to break it)
To help break this cycle, I used an 18 inch box to elevate her unaffected foot and force her into more normal hip flexion on the affected side in a pain free range. This seemed to work so we added this to the home program using a stair step and eliminated front step-downs altogether, choosing instead to focus on the side step-down in the 40-0 range if you will. I also added single leg soccer kicks (no ball) forward and in a crossing fashion to work on stability, strength and proprioceptive control.
The athlete returned on 12/31 and seemed to be progressing but still had discomfort with running. So, I felt she was not ready for full go as of yet. She also still had discomfort with short and long shuffles moving to the involved side. At this point, her mom wanted to know what I thought. about practice.
I advised her that player x needed to continue with strengthening 3x/week and try to ease back into jogging as able. She said the first indoor practice was coming up the week of 1/4. My thoughts? Indoor soccer fields and PF pain are a bad fit – period. But, I told her to let her daughter warm-up and do a few drills to get a feel for things.
The verdict? I got an email on Saturday saying she could not practice due to the same discomfort. Her next stop is back at the surgeon’s office for a closer look at the knee tomorrow. I will keep you posted on the diagnosis and treatment as this is an issue that all of us who work with athletes face and struggle with. Finding the right balance and progression between rest, rehab and return to play is tricky. So stay tuned for more details.



