Brian Schiff’s Blog
Injury Prevention, Sports Rehab & Performance Training Expert
High school baseball season is upon us. My son is a high school junior and recently verbally committed to pitch for a Division 1 school. He has worked hard to earn that offer, but the part most people do not see is the arm care and recovery work we do for him behind the scenes. Below is a recent picture of him in action.

I see lots of baseball players in my clinic ranging from 10 year olds to my MLB guys. One of the biggest issues I confront in my players (more commonly pitchers and catchers) is a condition known as internal impingement. While not the same thing as subacromial impingement, it still can impact the rotator cuff. Essentially, there is friction that causes irritation and in some cases injury to the rotator cuff and/or labrum. This usually manifests as pain in late cocking and the inability to throw hard without pain. Pitchers report decreased velocity and catchers struggle to thrown down to second with their their normal ease.
One of the most common issues leading to this is a loss of total shoulder motion on the throwing arm. Most notably, some players display significantly less internal rotation (IR) range of motion. Some loss of internal rotation is normal and expected over time provided they gain enough external rotation (ER) on the throwing side to counterbalance the asymmetry. Often, too much throwing early in the season or a big jump in pitch count/intensity/volume coupled with the ROM loss causes pain. This can occur suddenly or gradually build up over a few outings or games.
Search results for: internal impingement
Femoroacetabular impingement (FAI) is often a hidden and misunderstood cause of hip pain. I currently work with a physician who has studied under some of the best hip arthroscopists in the US, and he is performing arthroscopic procedures to resolve hip impingement. For many years, this has likely been a source of misdiagnosed, under treated and debilitating hip pain for people.
As things advance in medicine, hip arthroscopy is expanding and allowing for easier surgical correction of these issues. However, it is not an easy surgery technically speaking. As such, finding the right surgeon (if needed) is critical to attaining a positive outcome. Who normally gets it? Unfortunately, many people are predisposed to it, much like we see the natural genetic architecture (shape) of the acromion affecting impingement in the shoulder.
If you have an overhang of the hip acetabulum (socket) or non-spherical shape of the femoral head (or both) this can compromise the joint space and injure the joint cartilage and/or labrum. Destruction can occur at a very young age. I am currently rehabbing a 19 y/o male who recently underwent hip arthroscopy to debride his labrum and smooth out the hip socket and re-shape the femoral head. He had extensive damage at an early age due to his joint architecture and shows some signs of impingement on the other side as well.
How do you know if you have hip impingement? Generally, you may have hip joint pain along the front, side or back of the hip along with stiffness or a marked loss of motion (namely internal rotation). It is common in high level athletes and active individuals. However, other things may cause hip pain as well such as iliopsoas tendonitis, low back pain, SI joint pain, groin strain, hip dysplasia, etc. so a careful history, exam and plain films are necessary to confirm the diagnosis. If suspected, an MR athrogram is usually ordered to confirm if there are labral tears present. Physicians also use an injection with anesthetic to see if the pain is truly coming from the hip joint. This may be done under fluoroscopy to ensure it is in the joint space.
Signs and symptoms of FAI may include:
- Pain with sitting
- Pain or limited squatting
- Stiffness and decreased internal rotation
- Pain with impingement testing (see picture below of hip flexion, adduction and internal rotation – examiner will move the hip into this position and marked stiffness/loss of internal rotation and pain indicates a positive test)

Conservative treatment typically involves limiting or avoiding squats, strengthening the core and hip stabilizers as well as attempting to maximize mobility of the joint. Due to the fact that by the time pain brings patients in to see the doctor there has already been marked labral and joint damage, a cautious and proactive approach to managing hip pain is warranted especially in younger active patients and athletes.
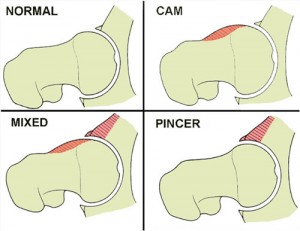
The types of lesions seen are either Cam or Pincer lesions.
Cam lesion – involves an aspherical shape of the femoral that causes abnormal contact between the ball and socket leading to impingement
Pincer lesion – involves excessive overgrowth of the acetabulum resulting in too much coverage of the femoral head and causing impingement where the labrum gets pinched
You can also see a mixed lesion where Cam and Pincer lesions are involved. FAI may lead or contribute to cartilage damage, labral tears, hyperlaxity, sports hernias, low back pain and early arthritis.
The good news is that these patients typically do well post-operatively. Dr. Philipon et al reported in 2007 in the Knee Surg Sports Traumatol Arthrosc. (click here to read the abstract) on 45 professional athletes who underwent arthroscopic management of FAI with an average follow-up of 1.6 years. In this time period 78% of them were able to return to their sport.
Following surgery, weight bearing may be restricted for the first 4 weeks or so to protect the labrum if it is repaired. With a simple debridement and re-contouring of the acetabulum, weight bearing may be initiated earlier. Avoiding twisting motions and excessive external rotation is a must in the first month or so as well. Typically, impact and twisting restrictions are lifted around 3 months post-op.
In the end, proper diagnosis and treatment is necessary to preserve the hip joint and maximize function and return to sport. If you or someone you know suffers from chronic and persistent hip pain that has failed conservative treatment, then consider getting a second look to rule out FAI.
Search results for: internal impingement
Whether you are lay person, trainer or therapist reading this blog, I try to keep you up to date on science, training and my interpretation/application of exercise based upon the research and practical application in my practice.
Today, I want to touch on an article just published in the Journal of American Sports Medicine. It was based on a study conducted by Tim Tyler et al in New York. They set out to determine what effect decreasing GIRD (aka glenohumeral internal rotation deficit) and posterior shoulder tightness had on reducing symptoms associated with internal shoulder impingement.
For those unfamiliar with GIRD, it basically looks at total shoulder motion side to side but focuses on deficits in internal rotation. Throwers often lack internal rotation on their dominant arms and exhibit excessive external range of motion for cocking and ball velocity. We tend to call this acquired laxity. Pitchers tend to have higher GIRD as well. Keep in mind total shoulder motion is critical as well. So, you cannot assume one will have problems just becasue there is decreased internal rotation.
You may see similar GIRD and psterior shoulder tightness patterns in other overhead athletes (swimmers, tennis players, volleyball players, etc.) This particular study looked at the effect on 11 men and 11 women who received manual mobilization by a PT combined with ER ROM, posterior shoulder stretches and scapular strengthening.
They studied all 22 subjects (range of symptoms from 1 to 24 months) and then compared data on the patients with and without symptom resolution. In effect the study revealed that posterior shoulder tightness was significantly improved in 12 of the subjects that had complete resolution of symptoms (more so than in the 10 who did not). In addition, changes in GIRD did not seek to impact the results.
What is the take away from this study? In a nutshell, if you have symptoms related to internal impingement, you should be doing posterior shoulder stretches. So, what are the best ones to do? There was a recent article in the NSCA Strength and Conditioning Journal (December 2009) that laid out some effective stretches (two of which I will show you in the video). Also, you should note that this pattern of tightness is common in weight lifters.
I have included a short video clip with 3 effective stretches that easily can be done at home. The stretches are as follows:
- Standing cross chest shoulder pull (across the chest) – this is a basic stretch I start most clients with who are experiencing pain. The drawback is that the scapula is not stabilized (or fixed) so you do not isolate the posterior shoulder effectively. However, it tends to be more comfortable for many early on and you will still get some benefit. When you are ready, it can be done against a wall to fix the scapula.
- Side lying cross chest shoulder pull – this would be equivalent to doing stretch number 1 against a wall. The floor acts to stabilize the scapula and then you pull the arm up and hold.
- The sleeper stretch – go easy with this one as pushing too hard may actually increase inflammation in my experience. You may also vary the angle of the upper arm to hit different portions of the joint capsule. For example, you may elect to stretch at 90, 70 and 45 degrees.
I advocate holding each stretch for 20-30 seconds and repeating 2-3 times daily. If you are in therapy, the stretching should be done following the joint mobilization by your therapist. Click the video below to see the stretches.
Search results for: internal impingement
Shoulder impingement is a common problem for many clients. Specifically, some clients will suffer from internal impingement as a result of a significant loss of internal rotation range of motion, also known as GIRD (glenohumeral internal rotation deficit). This has been widely researched in baseball players, and it is a common issue for overhead athletes. Of note, it can also impact those doing repetitive overhead lifts.
It is common to see asymmetry in internal range of motion for the dominant and non-dominant arms. For those clients who have a total shoulder motion asymmetry greater than 5 degrees, it becomes more important to resolve internal range of motion deficits based on the current literature. In my previous post, I revealed how to improve soft tissue mobility. In this post, I will review the sleeper stretch and cross body stretch to improve posterior shoulder mobility while increasing internal rotation.
The video below from my column ‘Functionally Fit’ for PFP Magazine will demonstrate how to do these stretches.
Search results for: internal impingement
Spring training has begun, and youth baseball players all over the country are starting to practice and prepare for their upcoming seasons. My very own 14 y/o son has started his 8th grade season, while having been working with his travel team on the weekends since mid December.
As a physical therapist, former player, father, and assistant coach on his 14U team, my first concern is always the health of a player. I see several baseball players in my sports medicine practice ranging in age from 9 year olds to MLB platers. Diagnoses include internal impingement, SLAP tears, little league elbow/shoulder, OCD, UCL sprains, rotator cuff tendinitis, instability, fractures and scapular dyskinesia.
One of the hardest things to do in my profession is get inside the head of a young athlete. Many will refrain from mentioning pain for fear of letting down a parent or coach, or out of concern for losing playing time. Society has become too focused on early specialization and winning from an early age. In addition, “travel baseball” has been somewhat diluted and water down by lots of dads who want their sons to play year-round. I often see kids being abused on terms of too little rest or improper recovery after they pitch and catch.
The biggest, most athletic and hardest throwing kids undergo the most strain as they are asked to shoulder the load at pitcher, catcher and shortstop early on. Many coaches are counting innings in tourneys and not pitches based on tournament guidelines. Too many kids are pitching on consecutive days without proper rest all in an attempt to win meaning less tournaments at a young age. Fortunately, we are making progress in the sports medicine world thanks to the efforts of Dr. James Andrews and others.
High schools are adopting pitch count regulations this year, and MLB along with Dr. Andrews has developed their site, www.pitchsmart.org, to spread education about injury prevention in youth pitchers. Dr. Christopher Ahmad is on the advisory committee for PitchSmart.org, and he is also the lead author on a new paper detailing an injury assessment tool for young baseball players, The Youth Throwing Score.